COVID-19 pandemic in India
This article needs to be updated. (April 2021) |
| COVID-19 pandemic in India | |||||||
|---|---|---|---|---|---|---|---|
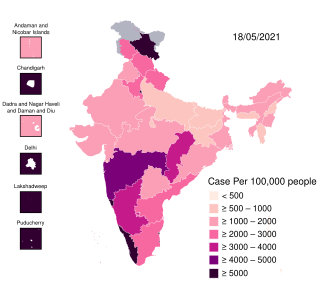 COVID-19 cases per 100,000 people by state, as of 18 May
| |||||||
| |||||||
| |||||||
| |||||||
| Disease | COVID-19 | ||||||
| Virus strain | SARS-CoV-2 | ||||||
| Location | India | ||||||
| First outbreak | Wuhan, Hubei, China[1] | ||||||
| Index case | Thrissur, Kerala[2] 10°31′39″N 76°12′52″E / 10.5276°N 76.2144°ECoordinates: 10°31′39″N 76°12′52″E / 10.5276°N 76.2144°E | ||||||
| Date | 30 January 2020 – ongoing (1 year, 4 months, 1 week and 6 days)[3] | ||||||
| Confirmed cases | 29,359,155 | ||||||
| Active cases | 1,080,690 | ||||||
| Recovered | 27,911,384 | ||||||
Deaths | 367,801 | ||||||
Territories | 28 states and 8 union territories[4] | ||||||
| Vaccinations | 249,600,304 | ||||||
| Government website | |||||||
| www www | |||||||
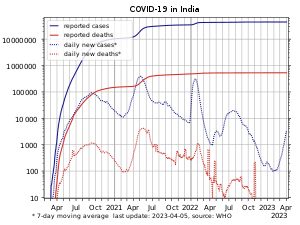
The COVID-19 pandemic in India is part of the worldwide pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first case of COVID-19 in India, which originated from China, was reported on 30 January 2020.[5] India currently has the largest number of confirmed cases in Asia.[6] As of 12 Jun 2021, India has the second-highest number of confirmed cases in the world (after the United States) with 29.3 million reported cases of COVID-19 infection and the third-highest number of COVID-19 deaths (after the United States and Brazil) at 367,081 deaths.[7][8][9]
The first cases of COVID-19 in India were reported in the towns of Thrissur, Alappuzha and Kasargod, all in the state of Kerala, among three Indian medical students who had returned from Wuhan.[10][11] Lockdowns were announced in Kerala on 23 March, and in the rest of the country on 25 March. By mid-May 2020, five cities accounted for around half of all reported cases in the country: Mumbai, Delhi, Ahmedabad, Chennai and Thane.[12] On 10 June, India's recoveries exceeded active cases for the first time.[13] Infection rates started to drop in September, along with the number of new and active cases.[14] Daily cases peaked mid-September with over 90,000 cases reported per-day, dropping to below 15,000 in January 2021.[15]
A second wave beginning in March 2021 was much larger than the first, with shortages of vaccines, hospital beds, oxygen cylinders and other medicines in parts of the country.[15] By late April, India led the world in new and active cases. On 30 April 2021, it became the first country to report over 400,000 new cases in a 24-hour period.[16][17] Health experts believe that India's figures have been underreported due to several factors.[17][18][19][20]
India began its vaccination programme on 16 January 2021, and by April was administering 3–4 million doses a day.[21][22] India has authorised the British Oxford–AstraZeneca vaccine (Covishield), the Indian BBV152 (Covaxin) vaccine, and the Russian Sputnik V vaccine for emergency use. As of 25 May 2021[update], the country had administered over 200 million vaccine doses.[23]
Timeline
2020
On 12 January 2020, the WHO confirmed that a novel coronavirus was the cause of a respiratory illness in a cluster of people in Wuhan, Hubei, China, which was reported to the WHO on 31 December 2019.[26]
On 30 January 2020, India reported its first case of COVID-19 in Thrissur, Kerala,[10] which rose to three cases by 3 February 2020; all were students returning from Wuhan.[27] Apart from these, no significant rise in transmissions was observed in February. On 4 March 22 new cases were reported, including 14 infected members of an Italian tourist group.[28] Transmissions increased over the month after several people with travel history to affected countries, and their contacts, tested positive. On 12 March, a 76-year-old man, with a travel history to Saudi Arabia, became the first COVID-19 fatality of India.[29]
A Sikh preacher, who had a travel history to Italy and Germany, turned into a superspreader by attending a Sikh festival in Anandpur Sahib during 10–12 March.[30][31][32] Over 40,000 people in 20 villages in Punjab were quarantined on 27 March to contain the spread.[31][33] On 31 March, a Tablighi Jamaat religious congregation event in Delhi, which had taken place earlier in March, emerged as a COVID-19 hotspot.[34][35][36] On 2 May, around 4,000 stranded pilgrims returned from Hazur Sahib in Nanded, Maharashtra to Punjab. Many of them tested positive, including 27 bus drivers and conductors who had been part of the transport arrangement.[37][38][39]
In July 2020, it was estimated based on antibody tests that at least 57% of the inhabitants of Mumbai's slums may have been infected with COVID-19 at some point.[40]
A government panel on COVID-19 stated in October 2020 that the pandemic had peaked in India, and could come under control by February 2021.[41] This prediction was based on a mathematical simulation referred to as the "Indian Supermodel", assuming that India reaches herd immunity.[42][43][44][45] That month, a new SARS-CoV-2 variant, Lineage B.1.617, was detected in the country.[46]
2021
India began its vaccination programme on 16 January 2021.[47] On 19 January 2021, nearly a year after the first reported case in the country, Lakshadweep became the last region of India to report its first case.[48] By February 2021, daily cases had fallen to 9,000 per-day.[49][50] However, by early-April 2021, a major second wave of infections took hold in the country; on 9 April, India surpassed 1 million active cases,[51] and by 12 April, India overtook Brazil as having the second-most COVID-19 cases worldwide.[52] By late April, India passed 2.5 million active cases and was reporting an average of 300,000 new cases and 2,000 deaths per-day. Some analysts feared this was an undercount.[53] On 30 April, India reported over 400,000 new cases and over 3,500 deaths in one day.[54]
Multiple factors have been proposed to have potentially contributed to the sudden spike in cases, including highly-infectious variants of concern such as Lineage B.1.617,[55][56] a lack of preparations as temporary hospitals were often dismantled after cases started to decline, and new facilities were not built,[57][58] and health and safety precautions being poorly-implemented or enforced during weddings,[59] festivals (such as Holi on 29 March,[60][61] and the Haridwar Kumbh Mela which was linked to linked to at least 1,700 positive cases between 10 and 14 April including cases in Hindu seers),[62][63] sporting events (such as IPL[64]), state and local elections in which politicians and activists have held in several states,[65] and in public places.[60][61] An economic slowdown put pressure on the government to lift restrictions,[66] and there had been a feeling of exceptionalism based on the hope that India's young population and childhood immunisation scheme would blunt the impact of the virus.[66] Models may have underestimated projected cases and deaths due to the under-reporting of cases in the country.[67][66]
Due to high demand, the vaccination programme began to be hit with supply issues; exports of the Oxford–AstraZeneca vaccine were suspended to meet domestic demand,[68] there have been shortages of the raw materials required to manufacture vaccines domestically,[69] while hesitancy and a lack of knowledge among poorer, rural communities has also impacted the programme.[68][47][50]
The second wave placed a major strain on the healthcare system,[60] including a shortage of liquid medical oxygen due to ignored warnings which began in the first wave itself,[70][71] logistic issues, and a lack of cryogenic tankers.[72][73][74][75] On 23 April, Modi met via videoconference with liquid oxygen suppliers, where he acknowledged the need to "provide solutions in a very short time", and acknowledged efforts such as increases in production, and the use of rail,[76] and air transport to deliver oxygen supplies.[77][78] A large number of new oxygen plants plants were announced;[79] the installation burden being shared by the center, coordination with foreign countries with regard to oxygen plants received in the form of aid, and DRDO.[80] A number of countries sent emergency aid to India in the form of oxygen supplies, medicines, raw material for vaccines and ventilators.[81][82][83][84] This reflected a policy shift in India; for the first time in 16 years had this kind of aid been accepted.[85][86]
The number of new cases had begun to steadily drop by late-May; on 25 May, the country reported 195,994 new cases—its lowest daily increase since 13 April. However, the mortality rate has remained high;[87] by 24 May, India recorded over 300,000 deaths attributed to COVID-19.[88] Around 100,000 deaths had occurred in the last 26 days, and 50,000 in the last 12.[8]
In May 2021, WHO declared that two variants first found in India will be referred to as 'Delta' and 'Kappa'.[89]
Response
Health care and testing
| Total samples tested[90] | 339,039,861 |
|---|---|
| Total positive cases | 27,718,520 |
| New samples tested | 2,070,508 |
| New Positive cases | 170,815 |
| New Positivity Rate | 8.24% |
| Total active cases | 2,227,540 |
| Total deaths | 322,364 |
| Total recovered cases | 25,168,616 |
| Total Doses administered[91] | 205,720,660 |
| People vaccinated 1st dose[92] | 161,850,092 |
| People vaccinated 2nd dose | 43,870,568 |
| As of 28 May 2021[21] | |
The Union Health Ministry's war room and policy making team in New Delhi decide how coronavirus should be tackled in the country, and consists of the ministry's Emergency Medical Response Unit, the Central Surveillance Unit (IDSP), the National Centre for Disease Control (NCDC) and experts from three government hospitals among others.[93] In March 2020, India's strategy was focused on cluster-containment, similar to how India contained previous epidemics, as well as "breaking the chain of transmission".[93][94] 52 labs were named capable of virus testing by 13 March.[95]
On 14 March 2020, scientists at the National Institute of Virology (NIV) isolated a strain of the novel coronavirus. India was the fifth country to successfully obtain a pure sample of the virus;[96] isolation of the virus would help towards expediting the development of drugs, vaccines and rapid diagnostic kits in the country.[97] NIV shared two SARS-CoV-2 genome sequences with GISAID.[98] In May, the NIV introduced another test kit for rapid testing.[99]
Initial testing

Initially, the labs tested samples only from those with a travel history to 12 countries designated as high-risk, or those who had come in contact with anyone testing positive for the coronavirus, or showing symptoms as per the government guidelines.[100][101] On 20 March 2020, the government decided to also include all pneumonia cases, regardless of travel or contact history.[102][103] On 9 April, ICMR further revised the testing strategy and allowed testing of the people showing symptoms for a week in the hotspot areas of the country, regardless of travel history or local contact to a patient.[104] While the health ministry claimed enough tests were being performed,[103] experts disagreed, saying that community transmission may go undetected.[105]
Expansion of tests
On 17 March 2020, the health ministry decided to allow accredited private pathology labs to test for COVID-19.[106][107][108] A person could get a COVID-19 test at a private lab after a qualified physician in a government facility recommended it.[109] Experts said this increased testing may ultimately result in a correction of the current under-counting and an increase in confirmed cases.[110]
111 additional labs for testing became functional on 21 March.[111] On 24 March, Mylab Discovery Solutions became the first Indian company to have received regulatory validation for its RT-PCR tests.[112][113] In April, Institute of Genomics and Integrative Biology, Delhi had developed a low cost paper-strip test that could detect COVID-19 within an hour. Each test would cost ₹500.00 (US$7.00).[114] On 13 April, ICMR advised pool testing in low infection areas to increase the capacity of the testing and save resources. In this process maximum five samples are tested at once and samples are tested individually only if a pool tests positive.[115] Faulty test kits from China were subsequently returned and future orders cancelled.[116][117][118][119]
By 9 July 2020, 1132 testing labs were functional. Following testing shortages, non-accredited private laboratories applying for accreditation were also given permission to test for coronavirus.[120] In September 2020, India had attained the highest number of daily tests in the world.[121] By 5 May 2021, 2506 testing labs (government and private) were functional and the total daily national testing capacity reached 1,500,000 tests.[122]
Testing community transmission
Testing for community transmission began on 15 March 2020. 65 government laboratories started testing random samples of people who exhibit flu-like symptoms and samples from patients without any travel history or contact with infected persons.[123][124] As of 18 March, no evidence of community transmission was found after results of 500 random samples tested negative.[125] Between 15 February and 2 April, 5,911 SARI (Severe Acute Respiratory Illnesses) patients were tested throughout the country of which, 104 tested positive (1.8%) in 20 states and union territories. About 40% of the identified patients did not have a travel history or any history of contact with a positive patient.[126] The ICMR advised to prioritise containment in the 36 districts of 15 states which had reported positive cases among SARI patients.[127]
In April 2020 WHO placed India in the community transmission stage however in June moved India to clusters of cases.[128] In October 2020, the health minister admitted to community transmission limited to some states and districts.[129] Until May 2021, India insisted that clusters of cases remained, and there was no nationwide community transmission.[130]
Daily samples tested
Daily new cases
New cases per day
Research and treatment


In Rajasthan, a combination of anti-malaria, anti-swine flu and anti-HIV drugs resulted in the recovery of three patients in March 2020.[131] On 23 March, the National Task Force for COVID-19 constituted by the ICMR recommended the use of hydroxychloroquine for the treatment of high-risk cases.[132][133]
In the same month, the Indian Institute of Chemical Technology, the Council of Scientific and Industrial Research (CSIR) and Cipla launched a joint venture to develop anti-COVID-19 drugs.[134][135] Another Indian firm, Stempeutics, announced plans to introduce a stem cell-based agent for treating critical COVID-19 patients;[136] the research will continue into 2021.[137] In April, funds for a number of preventive agents were released to initiate research.[138][139] The Centre for Cellular and Molecular Biology started working on genome sequencing of COVID-19 in early 2020.[140]
According to estimates, in March 2020 India had around 40,000 ventilators, of which 8,432 are with the public sector.[141] The government aimed to double the capacity of ventilators by June 2020,[142] with the assistance from Indian PSUs, firms and startups, including Bharat Electronics, DRDO and ISRO.[143][144][145][146] This led to the creation of some of the world's smallest and cheapest ventilators.[147]
Production lines have also been repurposed to manufacture general PPEs, full body suits and ventilators; from nil in near past, India was producing around 200,000 PPE kits and 250,000 N95 masks per day in May 2020.[148] By the second half of the month, India was the world's second largest producer of PPE body coveralls.[149]
Several states were allowed by ICMR and Drugs Controller General of India (DCGI) to start clinical trials of convalescent plasma therapy and plasma exchange therapy.[150][151][152] Initial optimism around plasma therapy,[153][154] resulted in ICMR stating that there is no robust evidence to support convalescent plasma therapy as a routine therapy, describing it is as an emerging and experimental therapy.[155] Convalescent plasma therapy was dropped form the covid-19 treatment protocol by ICMR in mid May 2021.[156][157]
In June 2020, India approved the repurposing of generic versions of the antiviral medication favipiravir for the treatment of mild-to-moderate COVID-19 symptoms by Glenmark, Cipla and the Indian Institute of Chemical Technology and Lupin Limited.[158][159][160] In July 2020, the Indian firm Biocon received emergency authorisation for the use of the repurposed drug Itolizumab in treatments for chronic plaque psoriasis, one of the symptoms of the disease.[161]
On 23 April 2021, Cadila Healthcare received an emergency authorisation to repurpose Peginterferon alfa-2b, a medication used to treat hepatitis C, as a treatment for moderate COVID-19 in adults.[162] On 8 May 2021, DCGI gave permission for emergency use of the drug 2-Deoxy-D-glucose developed by DRDO in collaboration with Dr. Reddy's Laboratories as an adjunct or alternative therapy for treating moderate to severe cases of COVID-19.[163]
Vaccine development and production
In January 2021, the DGCI initially approved the Oxford–AstraZeneca vaccine, manufactured by the Serum Institute of India (SII) under the trade name "Covishield",[164][165] and BBV152 (Covaxin), a vaccine developed by Bharat Biotech in association with the Indian Council of Medical Research and National Institute of Virology.[166]
The approval of Covaxin was met with some concern, as the vaccine had not then completed phase 3 trials.[167] Due to this status, those receiving Covaxin were required to sign a consent form,[168] while some states chose to relegate Covaxin to a "buffer stock" and primarily distribute the Oxford–AstraZeneca vaccine.[169] Following the conclusion of its trial, the DCGI issued a standard emergency use authorisation to Covaxin in March 2021.[170]
In April 2021, the DCGI approved the Russian Sputnik V vaccine, which was trialled in India by Dr. Reddy's Laboratories.[171][172] The initial shipment of 150 million Sputnik V doses arrived on 1 May, and began to be administered on 14 May.[173][174][175] Domestic manufacturing of Sputnik V is expected to begin by August 2021, with doses imported from Russia being used in the meantime.[176][177]
In May 2021, the DCGI approved phase 2 and 3 trials of Covaxin among children 2–18.[178]
Vaccination policy and distribution
- Top left: A healthcare worker administering a COVID-19 vaccine dose in AIIMS New Delhi on 16 January 2021.
- Top right: Frontline workers in Bihar filling COVID19 vaccination cards in May 2021.
- Bottom left:A COVID19 vaccination queue in Nagpur, Maharashtra on 1 May 2021.
India started out with a vaccination policy targeting 300 million people based on occupation and age group, to be completed a time period of six months, by August 2021.[179][180]
- Phase 1 started on 16 January 2021 and targeted 10 million health workers[a] first followed by 20 million frontline workers.[b][184][185] Phase 1 was to be completed by 31 March.[186][185] On 3 April, registrations for this group was closed.[187] 67% of health, frontline workers received at least one dose; taking into account registered health and frontline workers, the number of fully vaccinated is 47%.[186][188]
- Phase 2 began on 1 March 2021 to cover 45+ year old's with co-morbidities and 60+ year old's.[185] On 1 April, vaccinations were opened for everyone above 45 years.[185] Shortages in vaccine supplies were evident in March.[189]
On 19 March 2021, in the Lok Sabha, the health minister of India stated that "It is not necessary, scientifically, to give each and every person in the country the vaccine. Not each and every person in the world will be vaccinated. The prioritisation process is a dynamic process..."[190]
- Phase 3 of the vaccination campaign was opened up to include all eligible adults (18+) from 1 May 2021 following a surge in cases in April, a second wave.[191][186] This expansion resulted in immediate, increased and prolonged vaccine shortages.[180]
Changes in procurement policies, the liberalised vaccination policy,[192][191] and differential pricing further complicated the situation.[193][194] Global vaccine obligations of India were also severely affected including those with south-Asian neighbours,[195] and 190 countries associated with COVAX.[196][197]
Administratively India started preparing to vaccinate its population as early as April 2020 with the setting up a Vaccine Task Force.[198] Following this the National Expert Group on Vaccine Administration for COVID-19 (NEGVAC) was formed,[199] and in October 2020 states were asked to set up state level mechanisms for the COVID-19 vaccine programme,[200] and prepare cold chains points.[201][202] The government of India announced its COVID Suraksha Mission (transl. COVID Security Mission) in November 2020 by infusing ₹900 crore (US$130 million) into the Department of Biotechnology to aid the development of a COVID vaccine.[203] The 2021 budget of India also allocated ₹35,000 crore (US$4.9 billion) for vaccine procurement.[204] A communication strategy for the vaccination programme was also revealed by the health ministry in January 2021, targeting issues such as vaccine eagerness and hesitancy.[205] In a timeframe of one month, vaccine wastage across India was reduced from 10% to 5%.[206]
Immediate relief
Welfare
On 19 March 2020, Kerala announced a stimulus package of ₹20,000 crore (US$2.8 billion) to help the state overcome both the COVID-19 epidemic and economic hardship caused by it.[207] On 21 March, Uttar Pradesh announced ₹1,000 (US$14) to all daily wage labourers.[208] On 22 March, Punjab announced ₹3,000 (US$42) to all registered construction workers.[209] A number of states and union territories went on to announce free and increased rations for ration card holders.[210] Karnataka announced ₹1,610 crore (US$230 million) relief for unorganised sectors including flower growers, washer-men and women, barbers, construction workers, auto and cab drivers, MSMEs, and weavers.[211] The Delhi government announced that if a doctor, nurse or hygiene worker dies during treatment, their family will be provided ₹10 million (US$140,000).[212] The Union government also announced the distribution of rations.[213]
Economic relief and stimulus package
A food security scheme, part of wider economic relief package of ₹1.7 lakh crore (US$24 billion), was announced by the center on 26 March 2020. This also included direct cash transfer, primarily for migrant labourers and daily wage labourers; and free gas cylinders for three months.[214] This was followed by RBI cutting repo rates, injecting liquidity and permitting banks to provide a moratorium on all loans for three months.[215] Payment of taxes was relaxed and states were provided with short term credit via increased ways and means advances limits.[215] Pending wages of daily wage labourers under Mgnrega scheme were released.[216] On 12 May the Prime Minister announced an economic package of ₹20 lakh crore (US$280 billion); this included previous government actions, including the RBI announcements and the Finance Ministers announcement on 26 March.[217][218] On 12 October and 12 November, the government announced two more economic stimulus packages, bringing the total economic stimulus to ₹29.87 lakh crore (US$420 billion).[219] ₹15,000 crore (US$2.1 billion) was sanctioned for the health sectors response to COVID-19.[220]

Lockdowns
First wave: Nation-wide
The Epidemic Diseases Act, 1897 and Disaster Management Act, 2005 was invoked in mid-March 2020.[225][226] All commercial domestic and international flights were suspended in March.[227][215] A number of cities and states announced that they would restrict public gatherings, dine-in restaurants, or order the closure of various non-essential businesses through 31 March to slow the spread of COVID-19.[228] On 19 March 2020, Prime Minister Modi asked all Indians to observe a 14-hour Janata curfew ("people's curfew") on 22 March, and to thank essential workers by clapping or ringing bells at 5 p.m. outside their homes.[229][230] The curfew was used to evaluate the feasibility of a national lockdown.[231][232]
On 24 March, with 519 confirmed cases and 9 deaths in the country,[233] the Prime Minister announced that India would be placed under a "total lockdown" for at least three weeks. All non-critical businesses and services were ordered closed except for hospitals, grocery stores, and pharmacies, and there was a "total ban" on leaving the home for non-essential purposes. All public transport was suspended.[234][232]
On 16 April, districts were divided into zones using a colour-coded tier system based on incidence rates, classified as a "Red" (hotspot), "Orange", or "Green" (little to no transmission) zone. All of India's major cities fell into Red zones.[235][236] Beginning 20 April, agricultural businesses and stores selling farming supplies were allowed to resume operation, as well as public works programmes, cargo transport, and banks and government centres distributing benefits.[237] Phase 3[238] and 4 of the lockdown extended till 31 May, with incremental relaxations and changes.[239][240] The country began a phased lifting of restrictions on 8 June.[241] This phased lifting of restrictions continued in a series of "unlocks" which extended into November 2020.[227][242][243]
The government was criticised for not using the lockdown to prepare the health system for when the lockdown would be lifted.[244]
Second wave: State-wide and localised
Cities in Maharashtra such as Amravati and Nagpur started imposing curfew restrictions and lockdown measures in late February and early to mid-March 2021.[245][246] On 4 April, Maharashtra imposed a weekend lockdown and night curfew among other restrictions.[247] By early to mid-May, 35 of 36 of India's states and union territories had some form of state-wide and localised restriction.[248][249] The second wave of the pandemic in India has seen no nationwide lockdown.[248][249] Phased unlocking was announced starting June in Delhi, Tamil Nadu, Maharashtra, Uttar Pradesh and a number of other states.[250]
Administration, committees and task forces
India's covid response is being guided by a number of committees, empowered groups, advisory groups and task forces. Some of these were formed before the pandemic such as the National Technical Advisory Group on Immunisation (NTAGI), "India’s apex advisory body on immunization",[251] and the Integrated Disease Surveillance Programme (IDSP) under the National Centre for Disease Control.[252] IDSP was brought in as early as 17 January 2020.[253][254] Some of these were constituted following the onset of the pandemic such as the ICMR COVID-19 Task Force.[255] The National Expert Group on Vaccine Administration for COVID-19 (NEGVAC), formed in August 2020 would guide the national vaccine delivery strategy.[199] In October 2020, NEGVAC advice resulted in the formation of a three-tier state level mechanism for the implementation of the vaccine strategy.[200] The overall response has been led by the Prime Minister and his office; at least 67 review meetings have been held by it between January 2020 and May 2021.[252]
| Formation Date | Name | Members | Notes | Ref |
|---|---|---|---|---|
| 2020 | ||||
| 3 Feb | Group of Ministers (GOM) on COVID-19 | Chaired by Union Minister of Health and Family Welfare Harsh Vardhan | On 17 May 2021, the 26th meeting of the GOM was held. | [256][257] |
| 29 Mar | 11 Empowered Groups | Representatives from the Prime Minister's Office and the cabinet secretariat. Headed by Secretary level officers, NITI Aayog members including Amitabh Kant | Set up under Disaster Management Act 2005; 11 empowered groups set up to ensure quick decision making related to the pandemic and coordinate response. | [258] |
| 7 April | National Task Force for COVID-19 (ICMR COVID-19 Task Force) | Headed by VK Paul, Randeep Guleria and Balram Bhargava. | Set up by ICMR; terms of reference includes "identifying research priorities, review evidence, align research with level of outbreak and response; identify and create protocol; develop concept notes and identify partners for implementation". | [255][252] |
| 14 April | Vaccine Task Force | Co-chaired by VK Paul and PSA K. VijayRaghavan | Set up by the Prime Minister's Office; until 3 May 2021, 23 meetings of the VTF have been held. | [198] |
| ~31 May | National COVID-19 Supermodel Committee | M Vidyasagar, Manindra Agrawal, Lt Gen Madhuri Kanitkar, Biman Bagchi, Arup Bose, Gagandeep Kang, Sankar K Pal | Set up under the Department of Science and Technology; forecasting and modelling related to the pandemic. | [259] |
| 12 Aug | National Expert Group on Vaccine Administration for COVID-19 (NEGVAC) | Headed by VK Paul and Union Health Secretary Rajesh Bhushan | Vaccine delivery strategy. | [199][260] |
| 14 Sep | 6 Empowered Groups (reconstituted) | Headed by V.K. Paul, Guruprasad Mahapatra, Amitabh Kant, Tarun Bajaj, Ajay Bhalla | The 11 empowered groups set up on 29 March 2020 were reconstituted into 6 EGs. The groups had also undergone modification in May 2020. | [261][262][263] |
| 26 Oct | State Steering Committee. State/ District/ Urban/ Block Task Forces. | Chaired by Chief Secretary, Principal Secretary (Health), District Magistrate, Municipal Commissioner, SDM/ BDO respectively. | Following NEGVAC advice, the union government asked the states to form state-specific mechanisms in preparation for the implementation of the COVID-19 vaccination drive. | [200][264][265] |
| 25 Dec | Indian SARS-CoV-2 Consortium on Genomics (INSACOG) | Ten laboratories of Department of Biotechnology, MoST, CSIR, ICMR and MoHFW | "To monitor the genomic variations in the SARS-CoV-2 on a regular basis through a multi-laboratory network." | [266][267] |
| 2021 | ||||
| 9 May | National Task Force | Devi Shetty, Gagandeep Kang, Naresh Trehan, Saumitra Rawat, Shiv Kumar Sarin, Zarir Udwadia | Set up by the Supreme Court of India; "to facilitate a public health response to the pandemic based on scientific and specialised domain knowledge" and oxygen related issues. | [268] |
| Others: MoHFW's National Media Rapid Response Cell (NMRRC)[269] | ||||
Military
The Indian military has supported the Indian government's response during the pandemic.[270] During the second wave, some of the steps taken by the Indian military to help the fight against the pandemic includes setting up of COVID facilities,[271][272] setting up of oxygen PSA plants,[273] providing domestic and international air and water transport assistance,[273][270] providing medical assistance to civilians, providing nursing assistance and truck drivers,[270] providing support to centre and states as requested,[270] roping in retired military medics,[274] providing manpower with specialised skills,[275] and roping in the National Cadet Corps.[273] The three armed forces were functioning under Operation CO-JEET.[276] Operation Samudra Setu 1 which was officially conducted between 5 May 2020 and 8 July 2020 and focused on repatriation; and Samudra Setu 2 in 2021 focused on oxygen related transport.[277][278]
Private sector
In March–April 2020, several companies and organisations donated masks and other pandemic related supplies.[279][280][281] Several large business groups contributed to the PM CARES Fund.[282][283][284][285] Leading Indian corporates have come forward to provide support to hospitals across the country.[286] This includes procuring, setting up and maintaining cryogenic tanks, medical equipment and ventilators.[287] Business leaders in India have also set up COVID-19 facilities.[288] The chief executive officers of 40 US companies set up a global task force to collaborate on procuring equipment to support India.[289] Ola is providing doorstep delivery of medical oxygen.[290]
International support
The Indian government provided around 65.5 million doses of covid vaccines to 95 countries between 20 January 2021 and late March 2021. 10.5 million doses were gifted while the remaining were commercial and COVAX obligations.[291]
International support has been provided to India since the beginning of the pandemic in 2020.[292] In late April 2021, international relief being transported to India increased.[293] European countries such as France, Ireland, Belgium, Romania, Luxembourg, Portugal and Sweden sent pandemic related aid such as oxygen concentrators, ventilators and medicines.[294] France and Germany also sent oxygen plants; Germany also sent 12 army paramedics to operate the plants.[295][296] Oxygen related equipment was shipped from Bahrain, Thailand, Singapore[297] and Saudi Arabia.[298] Russia, United States of America and UNICEF sent various relief material including oxygen producing units.[299][292][300] In April 2021 Taiwan sent 150 oxygen machines to India. The oxygen machines had been purchased by the Taiwanese government and modified for India's electrical voltage.[301] Other countries to have provided support include Bhutan,[302] Bangladesh,[303] Kuwait,[304] Kenya,[305] Switzerland, Poland, Netherlands and Israel.[306] On 5 May 2021, Indian External Affairs Minister said that "What you describe as aid, we call friendship" in response to foreign support during the pandemic.[307] On 16 April, China sent 650,000 testing kits to India,[308] but their use was discontinued in view of a very low accuracy.[118][119]
There were international concerns related to how the support being sent to India is being used.[309][310] By 5 May India had received 5,769,442 items in aid.[311] Support between 27 April and 14 May included "10,796 oxygen concentrators, 12,269 oxygen cylinders; 19 oxygen generation plants; 6,497 ventilators, more than 4.2 lakh Remdesivir vials".[312] The government released the institutions and the states to which the support had been sent.[313][314][311]
Response shortages and criticism
The role of the National Centre for Disease Control during the COVID-19 pandemic has been questioned including the subdued sharing of data collected by the IDSP.[315] Disease surveillance in India through IDSP faces perpetual shortage of funds and manpower resulting in a weak nation-wide data collection system.[316] The IDSP does not track deaths taking place outside hospitals,[317] or deaths due to COVID-19 of those not tested,[318] one of the many reasons under-counting is built into the system. The lack of epidemiologists in senior decision making positions of COVID-19 related committees has been evident,[315] including the absence of state-level epidemiologists in a number of states.[319] In April 2020, the health ministry asked states to go on a hiring spree and fill vacancies for epidemiologists.[320] Indian Council of Medical Research has been criticised for did not updating the "treatment protocol for COVID-19" between July 2020 and April 2021.[321] The "National Task Force for COVID-19" did not meet during February and March despite members claiming it was obvious a second wave was in the making.[321] A number of warnings pertaining to a surge in cases in March, shortages in life-saving equipment and a second wave were downsized and went unheeded.[322] A number of problems were found with the forecasting and modelling by the National COVID-19 Supermodel Committee by independent commentators.[323] In early May 2021, the committee said that they hadn't been able to predict the second wave accurately.[324][325] A lot of problems with India's failing response to the second wave was the general and long term issues of the public health system in India.[316]
Preparations for another wave
The Principal Scientific Advisor to the Government of India said on 5 and 7 May 2021 that "Phase 3 is inevitable... it is not clear on what timescale this Phase 3 will occur... but we should prepare for new waves"[326][327] and that "If we take strong measures, a third wave may not happen... anywhere at all. It all depends on how well guidance is implemented at the local level, states, districts, cities."[328]
Studies into the origin of COVID-19
In April 2020, Indian officials stated that India was studying "all aspects" of the virus including its origins.[329] In May 2020 India supported an international push for an independent inquiry into the origins of COVID-19. The push for an inquiry was led by European Union and Australia and backed by 62 nations.[330] In November 2020, Chinese scientists claimed the virus originated in the Indian subcontinent.[331] In May 2021, India welcomed further studies into the origin of the disease.[332][333]
Impact
Displacement of migrant workers
The 2020 lockdown left tens of millions of migrant workers unemployed.[334][335] With factories and workplaces shut down, many migrant workers were left with no livelihood.[336] They thus decided to walk hundreds of kilometres to go back to their native villages, accompanied by their families in many cases.[337][338] In response, the central and state governments took various measures to help them.[339][340] The central government then announced that it had asked state governments to set up immediate relief camps for the migrant workers returning to their native states,[341] and later issued orders protecting the rights of the migrants.[342][343]
In its report to the Supreme Court of India on 30 March 2020, the central government stated that the migrant workers, apprehensive about their survival, moved in the panic created by fake news that the lockdown would last for more than three months.[344][345] In early May, the central government permitted the Indian Railways to launch "Shramik Special" trains for the migrant workers and others stranded,[346] but this move had its own complications.[347][348][349] On 26 May, the Supreme Court admitted that the problems of the migrants had still not been solved and ordered the Centre and States to provide free food, shelter and transport to stranded migrant workers.[350]
Drug shortages
In January 2020, Indian pharma companies raised the issue that drug supplies could be hit if the pandemic situation in China became worse.[351] India sources about 70% of its pharmaceutical ingredients from China.[352] In March 2020, India restricted export of 26 pharmaceutical ingredients; this restriction pointed to impending global shortages.[352] During the second wave of the pandemic in India shortages of certain drugs caused some COVID-19 patients to go to the black market.[353][354][355] In April 2021, other important COVID-19 related drugs also faced lowered stocks and sharp rise in cost of raw materials.[356][357]
Education
On 16 March 2020, the union government ordered the closure of schools and colleges.[358] On 18 March, Central Board of Secondary Education (CBSE) released revised guidelines for examination centers incorporating social distancing measures.[359] On 19 March, CBSE and JEE examinations for the Indian Institutes of Technology and other engineering college admissions were postponed.[360] States across the country postponed or cancelled school examinations; younger students were either automatically promoted or promoted based on prior performance.[361][362][363] The Union Public Service Commission also postponed the interview for the Civil Services Examination.[364] Only a few educational institutions in India have been able to effectively adapt to e-learning and remote learning; the digital divide is further impacted by serious electricity issues and lack of internet connectivity.[365][366][367]
Economy
Due to limited social movement restrictions during the second wave relative to lockdown measures during the first wave, the economic impact of the second wave to date is less severe than that of the first wave. Socio-economic indicators such as power demand, labour participation, and railway freight traffic fell less during the second wave as compared to the first wave.[368] The first wave has strengthened domestic economic resilience, visible during the second wave, despite the severity of the second wave.[369] The Indian Finance Ministry, in their Monthly Economic Review for April 2021 released on 7 May 2021, wrote that "economic activity has learnt to operate 'with Covid'".[370] Since the beginning of the pandemic in India, poverty has increased, and livelihoods have been affected.[371]
Indian stock markets witnessed a flash crash on 2 March 2020 on the back of the Union Health Ministry's announcement of two new confirmed cases.[372] On 12 March 2020, Indian stock markets suffered their worst crash since June 2017 after WHO's declaration of the outbreak as a pandemic.[373] On 23 March 2020, stock markets in India posted its worst losses in history.[374] SENSEX fell 4000 points (13.15%) and NSE NIFTY fell 1150 points (12.98%).[375] However, on 25 March 2020, one day after a complete 21-day lock-down was announced by the Prime Minister, SENSEX posted its biggest gains in over a decade.[376][377] The domestic stock markets have been in a positive rally from October 2020 to April 2021.[378]
Freedom of expression
On 25 April 2021 the government confirmed that it had made an emergency order requiring at least 100 social media posts to be removed by Facebook, Instagram, and Twitter, which included posts that it believed were misinformation, inducing panic among the public, or obstructing the response to the pandemic. This included critical tweets by West Bengal Minister of Labour and Law Moloy Ghatak, filmmaker and journalist Vinod Kapri, MP Revanth Reddy, and actor Viineet Kumar.[379][380][381]
On 30 April 2021, in a suo moto case regarding the government's response to the pandemic, a Supreme Court of India bench headed by Justice D Y Chandrachud commented on "free flow of information" and equated its restriction to contempt of court, "There should be free flow of information; we should hear voices of citizens. This is a national crisis. There should not be any presumption that the grievances raised on the internet are always false.[...] there should not be any kind of clampdown."[382]
On 21 May 2021, the Ministry of Electronics and Information Technology ordered social media outlets to remove all content that "names, refers to, or implies [an] 'Indian variant' of coronavirus", under the justification that it is misinformation because the World Health Organization does not officially recognise or use the term in relation to Lineage B.1.617.[383]
Health and other diseases
The attention given to fighting COVID-19 caused a reduction in attention given to other diseases such as tuberculosis, resulting in ten of thousands of deaths.[385] This has also caused a set-back to the fight against tuberculosis by over a decade.[386] The fall in tuberculosis registrations in the country fell 24% from 2019 to 2020 due to pandemic related issues.[387] Immunisation programs have been impacted, operations postponed and neglected and institutional delivery of babies decreased during the lockdown in 2020.[244]
Healthcare and frontline workers
On 8 August 2020, Indian Medical Association (IMA) announced that 198 doctors had died due to COVID-19.[388] This number was increased to 515 by October 2020,[389][390] and 734 by 3 February 2021.[391] However, on 2 and 5 February 2021 the health ministry announced in the Rajya Sabha and Lok Sabha respectively that 162/174 doctors, 107/116 nurses and 44 ASHA workers/199 healthcare workers had died due to COVID-19.[391][392] The figures were based on the governments "Insurance Scheme for Health Workers fighting COVID-19".[392] As of 17 April 2021, IMA put the number of deaths of doctors at 747.[393] Ten of thousands of doctors, nurses and health workers have been infected with covid.[394][393] Healthcare workers followed by frontline workers in India were provided with covid vaccinations first, starting from 16 January 2021.[395] This included 9,616,697 healthcare workers and 14,314,563 frontline workers; by May 2021 a majority of these had also been given their second dose.[396]
Religion

On 4 March 2020 the Prime Minister tweeted that he would not be participating in Holi programmes due to COVID-19.[397] The pandemic and subsequent lockdown resulted in numerous religious festivals being largely celebrated within homes or seeing less than normal public turnouts adhering to social distancing guidelines.[398] The Char Dham was conducted in a controlled manner; in 2020 pilgrims numbered 400,000 while the previous year had seen 3,800,000 pilgrims.[399][400] Many religious institutions adapted and connected to their devotees via livestreaming, radio and television.[401][402][403] Purported super-spreader events of a religious nature included the 2020 Tablighi Jamaat COVID-19 hotspot in Delhi,[404] and the 2021 Haridwar Kumbh Mela.[405] The state of Uttarakhand, where the Kumbh took place, saw a 1800% increase in COVID-19 during the period the Kumbh was held.[406][407] 2021 saw numerous religious events ignore social distancing guidelines such as Holi and Eid.[408][409]
Rural and semi-rural India
Over 70% of India's population, i.e. over 740 million people in India, live in rural areas.[410] The share of COVID cases in rural and semi-rural India increased from 40% in mid-July 2020 to 67% in August 2020.[411] This increase in covid cases was largely attributed to the movement of COVID infected migrant workers from urban areas back to their native villages.[411][412] Issues aggravating the situation in rural and semi-rural areas include a severe lack of human resources in the health field.[411] The second wave also saw migrants coming back from urbans areas, indicated by the sharp rise in employment generation through MGNREGS.[413] By May 2021, more than half the cases in Maharashtra and Uttar Pradesh were from rural areas.[414] Another indicator of the situation in villages is the rush of villagers to semi-urban and urban areas in search of healthcare, "about 30–35 per cent of the patients in hospitals in Bhopal are from villages and small towns located within a 200 km radius. It's the same story in Indore."[415] On 16 May 2021 a UP government official confirmed the report that corpses of people who succumbed to the virus in the rural areas had been dumped in the Ganges River due to lack of funds. Following this report, the UP state government announced that it will pay ₹5,000 (US$70) to poor families to cremate or bury the bodies of the dead.[416]
Transport
17 March 2020 onwards, private airlines such as IndiGo and Go Air started cancelling flights.[417][418] On 19 March, the Government of India announced that no international flights will be allowed to land in India from 22 March.[419] On 23 March, the union government announced the suspension of all domestic flights in the country starting 25 March.[420] Vande Bharat Mission, a mass evacuation program, was started by the government of India to repatriate 250,000 stranded Indians around the world.[421] On 7 August, Air India Express Flight 1344, a repatriation flight, crashed at Calicut International Airport, killing 18.[422] Two of the survivors tested positive for COVID-19.[423]
(Right) Quarantine and testing at Bengaluru Airport in April 2021.
Indian Railways took various initiatives to fight against the pandemic. Initially this included removing curtains and blankets from AC coaches,[424] hiking platform tickets,[425] and cancelling 3700 trains.[426] Metro services across India were suspended.[427] On 22 March, all train services in the country were cancelled baring goods trains, that is around 12,500 trains, and all non-essential passenger transport including interstate transport buses.[428][429] After Prime Minister Modi extended the nationwide lockdown to 3 May, Indian Railways suspended all services on its passenger trains and all ticket bookings indefinitely.[430] On 8 May, the Aurangabad railway accident occurred due to confusion related to the pandemic.[431] Public transport across the nation was affected.[432][433][434]
Other
In March 2020, there were several incidents of panic buying in India related to the pandemic.[435][436] Retailers and consumer goods firms saw their average daily sales more than double on 19 March as consumers rushed to buy essentials ahead of Modi's address to the nation.[437] Modi assured the citizens that there was enough food and ration supplies and advised them against panic buying.[438] The lockdown disrupted food supplies and threatened to trigger a food crisis.[439][440] By the first week of April, essential industries such as growing, harvesting and food deliveries were allowed to operate.[441]
A number of sporting events and fixtures in India were suspended, postponed or conducted behind closed doors such as the Indian Open badminton tournament,[442] I-League,[443] 2020 Indian Super League Final,[444][445] TCS World 10 Bengaluru, the IAAF Gold Label Road Race,[446] and a FIFA World Cup qualification match (India versus Qatar).[447] The 2020 ISSF World Cup, which was to commence on 15 March in New Delhi, was postponed.[448] On 13 March, the Board of Control for Cricket in India (BCCI) announced that the opening of the 2020 IPL was postponed from 29 March to 15 April; the tournament was eventually suspended indefinitely.[449][450] The IPL was eventually play in United Arab Emirates in September and November 2020.[451] BCCI also cancelled the ODI matches between India and South Africa on 15 and 18 March, which were originally announced to be played without spectators.[452]
From 7 March 2020, the Border Security Force decided to conduct the Wagah-Attari border ceremony without any spectators.[453] The Padma Awards ceremony, scheduled for 3 April 2020, was postponed.[454] On 17 March 2020, it was announced that all historical buildings in the country would remain closed to visitors;[455] the monuments were opened to the public on 6 July 2020.[456]
The International Indian Film Academy Awards, scheduled to take place on 27 March 2020, was cancelled.[457] Cinema halls were shut down; film bodies decided to stop the production of films, TV shows and web series till 31 March 2020.[458] On 25 March 2020, all major video streaming services in the country jointly announced that they would restrict streaming of high definition video on cellular networks during the 21-day lockdown, to preserve network capacity and infrastructure.[459]
Statistics
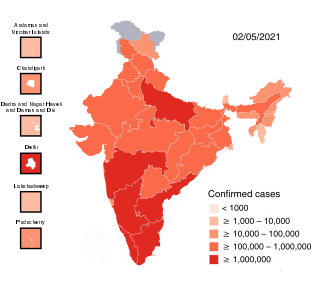
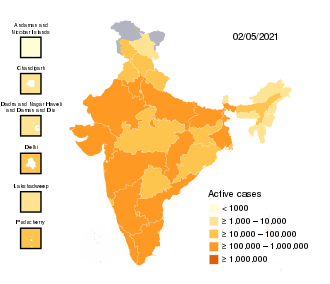
Cases have been reported in all states and union territories.[460]
Undercounting of cases and deaths
Undercounting of total cases and death figures was reported during the first wave in 2020. The discrepancies were detected by comparing official death counts released by the governments to the number of deaths reported in obituaries, at crematoria and burial grounds, etc. Some states were reported to have not added suspected cases to the final count contrary to WHO guidelines.[461][462][463] Similar undercounting was reported during the second wave in 2021.[464] There have been large gaps noted between official death figures and the sudden increase in the number of bodies being cremated and buried. Several crematoria that had been in disuse earlier were brought back into operation to keep up with the demand.[465][466] A series of articles in The Hindu newspaper estimated that compared to previous years, the number of additional deaths during the pandemic (known as the 'excess mortality') was about four times the official covid death toll in Chennai, Kolkata and Mumbai, and could be up to ten times higher in the state of Gujarat. However, it is not clear what proportion of these are due to covid and what are due to other factors such as overcrowding of medical facilities, lock-down, etc.[467]
See also
Notes
- ^ Health-care workers include "Health-care providers and workers in the health-care setting (public and private), including Integrated Child Development Services (ICDS) workers. The group has been further divided into nine sub-groups: medical officers, nurses and supervisors, frontline health and ICDS workers, paramedical staff, support staff, medical, nursing and paramedical students, medical scientists and research staff, clerical and administrative staff and other health staff."[181]
- ^ Frontline Workers (FLWs) include "Personnel from State and Central Police organisation, Armed Forces, Home Guards, prison staff, disaster management volunteers, Civil Defence organisation, Municipal Workers and revenue officials engaged in surveillance and containment activities."[181] A number of states have included journalists as frontline workers.[182] Gujarat has included crematorium workers as frontline workers.[183]
References
- ^ Sheikh, Knvul; Rabin, Roni Caryn (10 March 2020). "The Coronavirus: What Scientists Have Learned So Far". The New York Times. Retrieved 24 March 2020.
- ^ "Kerala confirmed first novel coronavirus case in India". India Today. 30 January 2020.
- ^ Reid, David (30 January 2020). "India confirms its first coronavirus case". CNBC. Retrieved 28 March 2020.
- ^ "Home | Ministry of Health and Family Welfare | GOI". mohfw.gov.in. Retrieved 12 June 2021.
- ^ Perappadan, Bindu Shajan (30 January 2020). "India's first coronavirus infection confirmed in Kerala". The Hindu. ISSN 0971-751X. Retrieved 24 February 2021.
- ^ "India most infected by Covid-19 among Asian countries, leaves Turkey behind". Hindustan Times. 29 May 2020. Retrieved 30 May 2020.
- ^ "#IndiaFightsCorona COVID-19". MyGov.in. Govt of India. Retrieved 12 June 2021.
- ^ a b Bhattacharya, Amit (24 May 2021). "India's Covid toll tops 3 lakh, 50,000 deaths in 12 days". The Times of India. Retrieved 24 May 2021.
- ^ "India's COVID crisis 'beyond heartbreaking': WHO". Al Jazeera. Retrieved 26 April 2021.
- ^ a b Andrews, MA; Areekal, Binu; Rajesh, KR; Krishnan, Jijith; Suryakala, R; Krishnan, Biju; Muraly, CP; Santhosh, PV (May 2020). "First confirmed case of COVID-19 infection in India: A case report". Indian Journal of Medical Research. 151 (5): 490–492. doi:10.4103/ijmr.IJMR_2131_20. PMC 7530459. PMID 32611918. Retrieved 1 June 2021.
- ^ Narasimhan, T. E. (30 January 2020). "India's first coronavirus case: Kerala student in Wuhan tested positive". Business Standard India. Archived from the original on 11 March 2020. Retrieved 7 March 2020.
- ^ "Infections over 1 lakh, five cities with half the cases: India's coronavirus story so far". The Week. Retrieved 20 May 2020.
- ^ Shivani Kumar (10 June 2020). "Covid-19: Number of recoveries exceed active cases for first time". Hindustan Times. New Delhi. Retrieved 11 June 2020.
- ^ "With very high COVID-19 testing, India's positivity rate fallen below 8%: MoHFW". The Economic Times. 18 October 2020. Retrieved 19 October 2020.
- ^ a b Michael Safi (21 April 2021). "India's shocking surge in Covid cases follows baffling decline". The Guardian. Retrieved 29 April 2021.
- ^ "Coronavirus | India becomes first country in the world to report over 4 lakh new cases on 30 April 2021". The Hindu. Special Correspondent. 30 April 2021. ISSN 0971-751X. Retrieved 2 May 2021.CS1 maint: others (link)
- ^ a b "India coronavirus: New record deaths as virus engulfs India". BBC News. 2 May 2021. Retrieved 3 May 2021.
- ^ Yeung, Jessie (28 April 2021). "As Covid sweeps India, experts say cases and deaths are going unreported". CNN.
- ^ Gettleman, Jeffrey; Yasir, Sameer; Kumar, Hari; Raj, Suhasini; Loke, Atul (24 April 2021). "As Covid-19 Devastates India, Deaths Go Undercounted". The New York Times. ISSN 0362-4331. Retrieved 3 May 2021.
- ^ "India COVID patients 'die due to oxygen shortage'". AL JAZEERA AND NEWS AGENCIES. 3 May 2021.
- ^ a b "#IndiaFightsCorona COVID-19". MyGov.in. 16 March 2020. Retrieved 18 February 2021.
- ^ Daily COVID-19 vaccine doses administered - India, Our World in Data. Retrieved 13 May 2021.
- ^ "200 million vaccine doses administered in India". Hindustan Times. 26 May 2021. Retrieved 26 May 2021.
- ^ "India's death toll soars past 10K, backlog deaths raise count by 437 in Delhi, 1,409 in Maharashtra". Hindustan Times. 17 June 2020. Retrieved 17 June 2020.
- ^ "45,720 new cases in 24 hrs, 13% positivity, single-day toll 1,129 after Tamil Nadu update". The Print. 23 July 2020. Retrieved 5 August 2020.
- ^ Reynolds, Matt (4 March 2020). "What is coronavirus and how close is it to becoming a pandemic?". Wired UK. ISSN 1357-0978. Archived from the original on 5 March 2020. Retrieved 5 March 2020.
- ^ Kumar, K. Reji (2020). "A comparative study of the SIR prediction models and disease control strategies: A case study of the state of Kerala, India". In Khalid Raza (ed.). Computational Intelligence Methods in COVID-19: Surveillance, Prevention, Prediction and Diagnosis. New Delhi: Springer. p. 166. ISBN 978-981-15-8533-3.
- ^ Perappadan, Bindu Shajan (4 March 2020). "COVID-19 | 6 members of Delhi patient's family test positive for coronavirus". The Hindu. ISSN 0971-751X. Retrieved 2 May 2020.
- ^ "India's first coronavirus death is confirmed in Karnataka". Hindustan Times. 12 March 2020. Retrieved 27 March 2020.
- ^ Wallen, Joe (28 March 2020). "40,000 Indians quarantined after 'super spreader' ignores government advice". The Telegraph. Retrieved 30 May 2021.
- ^ a b "Coronavirus: India 'super spreader' quarantines 40,000 people". BBC News. 27 March 2020. Retrieved 30 May 2021.
- ^ "Septuagenarian Sikh priest infected 27 of total 38 coronavirus cases in Punjab". India Today. Press Trust of India. 28 March 2020. Retrieved 30 May 2021.
- ^ Najib, Moska (29 March 2020). "At least 40,000 quarantined in India after single priest spread coronavirus". NBC News. Retrieved 30 May 2021.
- ^ Sharma, Neetu Chandra (18 April 2020). "30% covid-19 cases in India linked to Tablighi Jamaat event: Govt". Livemint. Retrieved 5 June 2020.
- ^ "India event sparks massive search for Covid-19 cases". BBC News. 31 March 2020. Retrieved 30 May 2021.
- ^ Kumar, Parimal (4 April 2020). Srinivasan, Chandrashekar (ed.). "30 Per Cent Of Coronavirus Cases Linked To Delhi Mosque Event: Government". With inputs from PTI. NDTV. Retrieved 30 May 2021.
- ^ "SAD, Congress leaders trade barbs as over 600 Nanded pilgrims contract coronavirus". The Times of India. Press Trust of India. 4 May 2020. Retrieved 4 May 2020.
- ^ "Punjab: 27 bus drivers & conductors that returned from Nanded test Corona positive". ABP News Live. 5 May 2020. Retrieved 6 May 2020.
- ^ "1,225 Nanded returnees test COVID-19 positive: government". The Hindu. 13 May 2020. ISSN 0971-751X. Retrieved 14 May 2020.
- ^ Hollingsworth, Julia; Mitra, Esha (29 July 2020). "More than half of Mumbai slum residents may have been infected with Covid-19, study suggests". CNN. Retrieved 23 February 2021.
- ^ Preeti Biswas (18 October 2020). "Covid-19 peak over; pandemic can be controlled by February 2021: Govt-appointed panel". The Times of India. Retrieved 19 October 2020.
- ^ Manindra Agrawal, Madhuri Kanitkar, M. Vidyasagar (October 2020), "Modelling the spread of SARS-CoV-2 pandemic - Impact of lockdowns & interventions", Indian Journal of Medical Research (in German), 153 (1 & 2), pp. 175–181, doi:10.4103/ijmr.IJMR_4051_20 (inactive 16 May 2021), PMID 33146155CS1 maint: multiple names: authors list (link) CS1 maint: DOI inactive as of May 2021 (link)
- ^ National Supermodel Committee. "Indian Supermodel for Covid-19 Pandemic" (PDF).
- ^ Super Model Committee. "National Supermodel of COVID-19 with Projections" (PDF).
- ^ "DST initiates COVID-19 India National Supermodel for monitoring infection transmission & aid decision-making by policymakers". Government of India, Ministry of Science and Technology.
- ^ "Expert reaction to cases of variant B.1.617 (the 'Indian variant') being investigated in the UK". Science Media Centre. Prof Sharon Peacock, University of Cambridge. 19 April 2021. Retrieved 20 April 2021.CS1 maint: others (link)
- ^ a b "Covid-19 vaccination: How is India's inoculation drive going". BBC News. 1 May 2021. Retrieved 22 April 2021.
- ^ "Nearly a year after Covid-19 outbreak in India, Lakshadweep reports its first-ever case". India Today. 19 January 2021. Retrieved 19 January 2021.
- ^ Yeung, Jessie; Sud, Vedika; Mitra, Esha (5 April 2021). "India reports new record of 103,558 daily Covid cases, as second wave and new lockdowns hit". CNN. Retrieved 22 April 2021.
- ^ a b Pandey, Vikas (7 April 2021). "India Covid-19: 'No end in sight' as doctors battle second wave". BBC News. Retrieved 22 April 2021.
- ^ Bhattacharya, Amit (10 April 2021). "Covid-19: Active cases cross 1 million, at all-time high now". The Times of India. Retrieved 12 April 2021.
- ^ "COVID-19: India overtakes Brazil with second highest number of cases". The New Indian Express. PTI. 12 April 2021. Retrieved 22 April 2021.CS1 maint: others (link)
- ^ Gettleman, Jeffrey; Yasir, Sameer; Kumar, Hari; Raj, Suhasini; Loke, Atul (24 April 2021). "As Covid-19 Devastates India, Deaths Go Undercounted". The New York Times. ISSN 0362-4331. Retrieved 24 April 2021.
- ^ Hollingsworth, Julia; McKeehan, Brett; Kottasová, Ivana (1 May 2021). "India records more than 400,000 Covid-19 cases in a single day". CNN. Retrieved 1 May 2021.
- ^ Rogers, Katie (25 April 2021). "Despite a billion vaccine shots given, Covid-19 runs rampant in much of the world". The New York Times. Retrieved 28 April 2021.
- ^ "India's 'double mutation' covid virus variant is worrying the world". mint. Bloomberg. 19 April 2021. Retrieved 28 April 2021.CS1 maint: others (link)
- ^ "State after state shut down special Covid centres just before second wave". The Indian Express. 26 April 2021. Retrieved 30 April 2021.
- ^ "India's COVID-19 emergency". The Lancet. 397 (10286): 1683. 8 May 2021. doi:10.1016/S0140-6736(21)01052-7. PMC 8102046. PMID 33965073.
- ^ "Superspreader events like weddings behind new Covid surge: Govt panel". Hindustan Times. 19 March 2021. Retrieved 30 May 2021.
- ^ a b c "Despite surge in cases, Covid guidelines flouted during Holi celebrations". The Indian Express. 29 March 2021. Retrieved 24 April 2021.
- ^ a b "Holi 2021: Scores of devotees flout COVID-19 protocols at Mathura's Dwarkadhish Temple". DNA India. 29 March 2021. Retrieved 25 April 2021.
- ^ Kamal, Hassan (22 April 2021). "Kumbh Mela and election rallies: How two super spreader events have contributed to India's massive second wave of COVID-19 cases". Firstpost. Retrieved 25 April 2021.
- ^ "Over 1,700 test positive for COVID-19 in Kumbh Mela over 5-day period". The Hindu. 15 April 2021. Retrieved 18 April 2021.
- ^ Anand Vasu (4 May 2021). "The IPL failed by ignoring stark warning signs of India's Covid crisis". The Guardian. Retrieved 5 May 2021.
- ^
- Arun Janardhanan (27 April 2021). "Irresponsible… must perhaps face murder charge: Madras HC on Election Commission". The Indian Express. Chennai. Retrieved 30 April 2021.
- "UP: After Report Says 135 People on Poll Duty Died Due to COVID-19, High Court Pulls Up SEC". The Wire. New Delhi. 27 April 2021. Retrieved 30 April 2021.
- Pandey, Neelam (13 April 2021). "Modi, Shah, Mamata or Rahul, no one cares about EC Covid warning & rallies continue as usual". ThePrint. Retrieved 27 May 2021.
- Jacob, Jeemon (7 April 2021). "Kerala: Elections to blame for Covid-19 spike". India Today. Retrieved 4 May 2021.
- Blair, Alex (28 April 2021). "Indian government criticised for praising political rallies midway through COVID-19 second wave". News AU. Retrieved 2 May 2021.
- Ghosh, Abantika (24 March 2021). "Punjab blames comorbidities, 'roster' of protesting farmers for Covid surge, Centre disagrees". ThePrint. Retrieved 27 May 2021.
- ^ a b c Safi, Michael (29 April 2021). "'We are not special': how triumphalism led India to Covid-19 disaster". The Guardian. Retrieved 30 April 2021.
- ^ Beaumont, Peter (22 April 2021). "Covid-19: India's response to second wave is warning to other countries". The Guardian. Retrieved 30 April 2021.
- ^ a b Beaumont, Peter (24 March 2021). "Delhi reportedly halts AstraZeneca Covid vaccine exports as cases soar". The Guardian. Retrieved 22 April 2021.
- ^ Yeung, Jessie; Suri, Manveena (1 May 2021). "Every adult in India is now eligible for Covid vaccine shots, but some states say they have none to offer". CNN. Retrieved 1 May 2021.
- ^ Patel, Anand (25 April 2021). "Parliamentary panel had alerted about oxygen shortage in February, says Congress". India Today. Retrieved 6 June 2021.
- ^ "Karnataka government ignored experts' advice to up oxygen supply". The New Indian Express. 20 August 2020. Retrieved 6 June 2021.
- ^ Ellis-Petersen, Hannah; Rourke, Alison (26 April 2021). "India's Covid crisis: doctors sound warning over oxygen hoarding". The Guardian. Retrieved 26 April 2021.
- ^ "Three reasons behind India facing an acute oxygen crisis". mint. Reuters. 24 April 2021. Retrieved 26 April 2021.CS1 maint: others (link)
- ^ Yeung, Jessie; Sud, Vedika (21 April 2021). "India's second Covid wave hits like a 'tsunami' as hospitals buckle under weight". CNN. Retrieved 22 April 2021.
- ^ Gettleman, Jeffrey; Raj, Suhasini; Kumar, Hari (21 April 2021). "India's Health System Cracks Under the Strain as Coronavirus Cases Surge". The New York Times. ISSN 0362-4331. Retrieved 22 April 2021.
- ^ "Covid-19: Railways runs its first Oxygen Express for loading Liquid Medical Oxygen". The Economic Times. 19 April 2021. Retrieved 26 April 2021.
- ^ "'Challenge is to provide solutions in a very short time': PM to oxygen producers". mint. 23 April 2021. Retrieved 26 April 2021.
- ^ Rai, Arpan (23 April 2021). "'Utilise full potential': PM Modi in meeting to review supply of medical oxygen". Hindustan Times. Retrieved 26 April 2021.
- ^ "Surge hits a new peak, Centre approves 551 oxygen plants for govt hospitals in districts". The Indian Express. 26 April 2021. Retrieved 26 April 2021.
- ^ Goswami, Sweta (9 May 2021). "Eight oxygen plants added in govt hospitals in Delhi in two weeks". Hindustan Times. Retrieved 6 June 2021.
- ^ "India's coronavirus crisis intensifies as cases hit new record". Raidió Teilifís Éireann. 26 April 2021. Retrieved 27 April 2021.
- ^ "Covid: Countries send aid to ease India's oxygen emergency". BBC News. 25 April 2021. Retrieved 26 April 2021.
- ^ Rogers, Katie (25 April 2021). "In Reversal, U.S. Will Send Vaccine Materials to Stricken India". The New York Times. ISSN 0362-4331. Retrieved 26 April 2021.
- ^ Sengupta, Somini (24 April 2021). "U.S. Is Under Pressure to Export More Vaccine Supplies Amid India's Deadly Surge". The New York Times. ISSN 0362-4331. Retrieved 3 May 2021.
- ^ Roy, Shubhajit (29 April 2021). "First policy shift in 16 yrs: India open to foreign aid, ok to buying from China". The Indian Express. New Delhi. Retrieved 1 May 2021.
- ^ Otukho, Jackson (29 April 2021). "India Pushed to Accept Foreign Aid for First Time in 16 Years as COVID-19 Cases Spike". Tuko. Retrieved 1 May 2021.
- ^ Bhattacharya, Amit (25 May 2021). "Coronavirus cases in India: After 40 days, daily Covid cases fall below 2 lakh". The Times of India. Retrieved 26 May 2021.
- ^ Mackintosh, Eliza (24 May 2021). "India's Covid deaths top 300,000". CNN. Retrieved 24 May 2021.
- ^ "COVID Variants Found in India to Be Labelled 'Delta', 'Kappa': WHO". TheQuint. 31 May 2021. Retrieved 6 June 2021.
- ^ "Indian Council of Medical Research, New Delhi". icmr.gov.in. Retrieved 18 February 2021.
- ^ "COWIN". COWIN Vaccine Dashboard. 27 May 2021.
- ^ "MoHFW | Home". www.mohfw.gov.in. Retrieved 18 February 2021.
- ^ a b Sharma, Sanchita (5 March 2020). "How conference hall at health ministry emerged as coronavirus-control war-room". Hindustan Times. Archived from the original on 7 March 2020. Retrieved 7 March 2020.
- ^ "Delhi declares coronavirus as epidemic as India reports first death from infection". The Week. 13 March 2020. Retrieved 13 March 2020.
- ^ "Coronavirus test in India: Complete list of testing sites for coronavirus in India". The Times of India. 13 March 2020. Retrieved 11 November 2020.
- ^ Jha, Durgesh Nandan (14 March 2020). "Coronavirus cases in India: Fewer cases, but India becomes 5th country to isolate coronavirus". The Times of India. Retrieved 14 March 2020.
- ^ Sharma, Neetu Chandra (13 March 2020). "India becomes fifth country to isolate Covid-19 virus strain". Livemint. Retrieved 14 March 2020.
- ^ Prasad, R. (7 March 2020). "Coronavirus | India shares two SARS-CoV-2 genome sequences". The Hindu. ISSN 0971-751X. Archived from the original on 7 March 2020. Retrieved 7 March 2020.
- ^ "National Institute of Virology develops 1st indigenous Elisa test kit for Covid-19: Harsh Vardhan". The Times of India. Press Trust of India. 10 May 2020. Retrieved 11 May 2020.
- ^ Kaul, Rhythma (15 March 2020). "India needs a more aggressive testing regimen for coronavirus: Experts". Hindustan Times. Retrieved 15 March 2020.
- ^ Krishnan, Vidya (13 March 2020). "Public-health experts raise concerns about India's restricted testing for COVID-19". The Caravan. Retrieved 15 March 2020.
- ^ Ghosh, Abantika (21 March 2020). "Covid-19 testing in India extended to all pneumonia cases: Govt". The Indian Express. Retrieved 21 March 2020.
- ^ a b "First and second confirmatory tests for COVID-19 are free: Sanjeeva Kumar". ANI News. 15 March 2020. Retrieved 18 March 2020.
- ^ Gunasekar, Arvind (9 April 2020). Sanyal, Anindita (ed.). "Coronavirus Testing Strategy Revised in India, Ambit Widened". NDTV. Retrieved 10 April 2020.
- ^ "Is India testing enough for coronavirus cases?". Scroll.in. 14 March 2020. Retrieved 15 March 2020.
- ^ Jha, Durgesh Nandan (17 March 2020). "Coronavirus testing lab: Accredited private labs to be allowed to test for Covid-19". The Times of India. Retrieved 17 March 2020.
- ^ Porecha, Maitri (17 March 2020). "Metropolis among private labs short-listed for coronavirus testing". The Hindu.
- ^ "Roche Diagnostics India first private firm to get COVID-19 test approval". India Today. PTI. 18 March 2020. Retrieved 29 May 2021.CS1 maint: others (link)
- ^ Ray, Kalyan (17 March 2020). "Health Ministry to allow accredited private labs to conduct tests for coronavirus". Deccan Herald. Retrieved 29 May 2021.
- ^ "India must prepare for a tsunami of cases". Sanjay Ganguly. BBC. 19 March 2020. Retrieved 20 March 2020.CS1 maint: others (link)
- ^ "111 labs for testing coronavirus will be functional across India from today: Health Ministry". India Today. ANI. 21 March 2020. Retrieved 29 May 2021.
- ^ Rajagopal, Divya (24 March 2020). "Pune based Mylab becomes first Indian company to get Covid-19 test kits validated". The Economic Times. PTI. Retrieved 29 May 2021.
- ^ Soni, Preeti (24 March 2020). "India can double coronavirus test kits to 200,000 in a week, thanks to Pune-based Mylabs". Business Standard. Retrieved 29 May 2021.
- ^ Choudhury, Srishti (2 April 2020). "India's first paper-strip test for Covid-19, CSIR lab makes a breakthrough". LiveMint. Retrieved 5 April 2020.
- ^ Chanda, Himani (13 April 2020). "ICMR advises 'pool testing' in low-infection areas to increase number of Covid-19 tests". ThePrint. Retrieved 15 April 2020.
- ^ "China dispatches 6.5 lakh medical kits to India to fight coronavirus". India Today. Press Trust of India. 16 April 2020. Retrieved 22 April 2020.
- ^ Singh, Shiv Sahay (20 April 2020). "NICED admits testing kits have problem in West Bengal". The Hindu. ISSN 0971-751X. Retrieved 21 April 2020.
- ^ a b "Coronavirus: India cancels order for 'faulty' China rapid test kits". BBC News. 28 April 2020. Retrieved 28 April 2020.
- ^ a b Porecha, Maitri (27 April 2020). "States asked to return faulty Chinese kits". The Hindu @businessline. Retrieved 28 April 2020.
- ^ Dutta, Sumi Sukanya (9 July 2020). "ICMR allows non-accredited private labs to carry out Covid-19 tests". The New Indian Express. Retrieved 9 June 2021.
- ^ Harshit Sabbarwal (3 September 2020). "India's Covid-19 tests per day highest in the world, says health ministry". Hindustan Times. New Delhi. Retrieved 19 October 2020.
- ^ Press Trust of India (5 May 2021). "India's COVID-19 crisis: ICMR revises RT-PCR testing guidelines to reduce pressure on diagnostic labs". Firstpost. Retrieved 9 June 2021.CS1 maint: uses authors parameter (link)
- ^ Patel, Shivam (14 March 2020). "ICMR to test for community transmission of Covid-19". The Indian Express. Retrieved 17 March 2020.
- ^ Thacker, Teena (17 March 2020). "Will know if India is going through community transmission of Covid-19: ICMR". The Economic Times. Retrieved 17 March 2020.
- ^ "Covid-19 outbreak: No evidence of community transmission, says ICMR". The Economic Times. 18 March 2020. Retrieved 18 March 2020.
- ^ Sharma, Milan (10 April 2020). "Coronavirus: Second ICMR report on random sampling test results shows possible community transmission". India Today. Retrieved 13 April 2020.
- ^ Press Trust of India (10 April 2020). "ICMR suggests containment in 36 districts after many with respiratory infection test Covid-19 positive". India Today. Retrieved 13 April 2020.CS1 maint: uses authors parameter (link)
- ^ Shankar, Abhishek; Saini, Deepak (25 August 2020). Dasson, Bharvi (ed.). "Centre's Stand on Community Transmission Amid Rising Covid-19 Cases Raises Planning Concerns". News18. Retrieved 12 June 2021.
- ^ Sharma, Neetu Chandra (19 October 2020). "India is in throes of community transmission, admits Vardhan". mint. Retrieved 12 June 2021.
- ^ "Despite record number of Covid cases, India continues to avoid community transmission tag". Scroll.in. 14 May 2021. Retrieved 12 June 2021.
- ^ "Combination of two anti-HIV drugs proved crucial in Coronavirus treatment, Rajasthan official". The Economic Times. Press Trust of India. 16 March 2020. Retrieved 22 March 2020.
- ^ Advisory on the use of hydroxy-chloroquine as prophylaxis for SARS-CoV-2 infection. National Task Force for COVID-19, Indian Council of Medical Research, Ministry of Health and Family Welfare. 22 March 2021. Archived on 14 January 2021.
- ^ Acharjee, Sonali (24 March 2020). "Covid-19: The bitter truth about using hydroxychloroquine as a preventive drug". India Today. Retrieved 29 May 2021.
- ^ "Health: CSIR-IICT ties up with Cipla to develop anti-COVID-19 drug". The Economic Times. Press Trust of India. 18 March 2020. Retrieved 22 March 2020.
- ^ "Cipla confirms collaboration with CSIR, IICT, ICMR to develop COVID-19 treatment-Health News , Firstpost". Firstpost. PTI. 5 August 2020. Retrieved 29 May 2021.CS1 maint: others (link)
- ^ Giriprakash, K (9 April 2020). "Stempeutics ties up with a consortium of stem cell firms for end-stage Covid-19 treatment". Business Line. Retrieved 23 March 2020.
- ^ Das, Sanjiv (3 May 2020). "We are in touch with CDSCO, will submit clinical trial protocol for approval of COVID-19 treatment". Express Pharma. Retrieved 29 May 2021.
- ^ Indian Ministry of Science and Technology (8 April 2020). "DST approves funding for developing a gel for nasal passage as prevention for COVID 19". Press Information bureau. Retrieved 13 April 2020.
- ^ Indian Ministry of Science and Technology (9 April 2020). "SCTIMST scientists design super absorbent material for safe management of infected respiratory secretions". Press Information bureau. Retrieved 13 April 2020.
- ^ Ramesh, M (26 March 2020). "CSIR lab working on genome sequencing of Covid-19". Business Line. Retrieved 13 April 2020.
- ^ Chandna, Himani (27 March 2020). "India has 40,000 ventilators but could need many, many more in 'worst-case scenario'". ThePrint. Retrieved 15 April 2020.
- ^ "India to double number of ventilators by making 40,000 units: Reports". The Week. 28 March 2020. Retrieved 15 April 2020.
- ^ Prasad, Nikita (6 April 2020). "Kudos! Indian Railways manufactures low-cost ventilator prototype for COVID-19 patients in a week's time". The Financial Express. Retrieved 6 April 2020.
- ^ Datti, Sharmishte (31 March 2020). "ISRO Puts Rockets, Satellites On Hold To Develop Ventilators For Coronavirus". GizBot. Retrieved 6 April 2020.
- ^ Pubby, Manu (4 April 2020). "Low cost, high volume products being developed; DRDO chief says scientists rising to the occasion". The Economic Times. Retrieved 6 April 2020.
- ^ Shukla, Archana (23 March 2020). "Bengaluru-based Skanray aims to make 1 lakh ventilators, opens up design IP". CNBC TV18. Retrieved 13 April 2020.
- ^ Jha, Kundan (11 April 2020). "India using innovation as arsenal to fight coronavirus". The Sunday Guardian. Retrieved 13 April 2020.
- ^ "From zero, India now produces around 2 lakh PPE kits per day". The Times of India. ANI. 5 May 2020. Retrieved 11 May 2020.
- ^ "India becomes world's second largest manufacturer of PPE body coveralls: Centre". The Times of India. Press Trust of India. 21 May 2020. Retrieved 23 May 2020.
- ^ Yadavar, Swagata (15 April 2020). "ICMR plans plasma therapy clinical trials in 2 weeks to treat critical Covid-19 cases". ThePrint. Retrieved 24 April 2020.
- ^ PTI (18 April 2020). "ICMR gets nod for clinical trial of convalescent plasma for COVID-19 treatment". The Hindu. ISSN 0971-751X. Retrieved 24 April 2020.
- ^ "Karnataka gets Centre's nod to start plasma therapy for COVID-19 patients". Livemint. 21 April 2020. Retrieved 24 April 2020.
- ^ Dwivedi, Sukirti (20 April 2020). "Plasma Therapy For COVID-19 Works in Delhi, 49-year-old Recovers". NDTV.
- ^ "Plasma therapy shows positive results on COVID-19 patients, says Kejriwal". Livemint. 24 April 2020. Retrieved 24 April 2020.
- ^ "No approved, definitive therapies for COVID-19; convalescent plasma one of several emerging therapies: ICMR". ANI News. Retrieved 28 April 2020.
- ^ "ICMR Removes 'Plasma Therapy' From COVID-19 Management Protocols". The Wire Science. 18 May 2021. Retrieved 27 May 2021.
- ^ "ICMR drops plasma therapy from COVID-19 treatment guidelines". The Hindu. Special Correspondent. 17 May 2021. ISSN 0971-751X. Retrieved 27 May 2021.CS1 maint: others (link)
- ^ "Glenmark's FabiFlu approved for coronavirus treatment in India, costs Rs 103 per tablet". India Today. 20 June 2020. Retrieved 30 June 2020.
- ^ Leo, Leroy (24 July 2020). "Cipla to launch favipiravir under Ciplenza in August at 68 rupees per pill". Livemint. Retrieved 4 August 2020.
- ^ "Lupin launches Covid-19 drug Favipiravir in India at Rs 49 per tablet". The Times of India. Press Trust of India. 5 August 2020. Retrieved 5 August 2020.
- ^ Leo, Leroy (11 July 2020). "Biocon Biologics' itolizumab gets DCGI nod for emergency use to treat covid-19". Livemint. Retrieved 28 April 2021.
- ^ "India's Cadila gets approval to repurpose Hepatitis C drug for Covid-19". Hindustan Times. 23 April 2021. Retrieved 24 April 2021.
- ^ "Easy to produce, easier to consume: DRDO's 2-DG drug for treatment of Covid patients | FAQs". India Today. 8 May 2021. Retrieved 13 May 2021.
- ^ Schmall, Emily; Yasir, Sameer (3 January 2021). "India Approves Oxford-AstraZeneca Covid-19 Vaccine and 1 Other". The New York Times.
- ^ "Coronavirus: India approves vaccines from Bharat Biotech and Oxford/AstraZeneca". BBC News. 3 January 2021. Retrieved 5 June 2021.
- ^ "Expert panel recommends Bharat Biotech's Covaxin for restricted emergency use". News18. 2 January 2021. Retrieved 5 June 2021.
- ^ Prasad, R (15 January 2020). "Vaccine dilemma — to take or not to take Covaxin". The Hindu. Chennai.
- ^ Bindu Shajan Perappadan (16 January 2020). "Covaxin recipients asked to sign consent form on 'clinical trial mode'". The Hindu. New Delhi. Retrieved 5 June 2021.
- ^ Prasad, R (15 January 2020). "Vaccine dilemma — to take or not to take Covaxin". The Hindu. Chennai. Retrieved 5 June 2021.
- ^ Leo, Leroy (11 March 2021). "DCGI removes Covaxin out of 'clinical trial mode'". mint. Retrieved 13 May 2021.
- ^ Som, Vishnu (13 April 2021). "On Sputnik V For India, Price Issues - AstraZeneca Price Too Low, Says Maker". NDTV. Retrieved 28 May 2021.
- ^ Saxena, Sparshita, ed. (16 September 2020). "Russia's sovereign wealth fund partners with Dr Reddy's for trials and distribution of Sputnik V vaccine in India". Hindustan Times. Retrieved 24 May 2021.
- ^ Watch: Russia's Sputnik V, 3rd Vaccine For India, Arrives In Hyderabad, NDTV, 1 May 201
- ^ "1.5 lakh doses of Sputnik V land in India", The Hindu, 1 May 2021
- ^ Kumar, N. Ravi (14 May 2021). "Sputnik roll out begins, to cost ₹995 per dose". The Hindu. ISSN 0971-751X. Retrieved 15 May 2021.
- ^ "On Sputnik V For India, Price Issues - AstraZeneca Price Too Low, Says Maker". NDTV.com. Retrieved 28 May 2021.
- ^ "Sputnik V Covid-19 vaccine production in India to start in August". The Times of India. New Delhi. 22 May 2021. Retrieved 25 May 2021.
- ^ "DCGI approves Covaxin clinical trials for children aged 2-18 years". DNA India. 13 May 2021. Retrieved 13 May 2021.
- ^ "India rolls out the world's largest COVID-19 vaccination drive". World Health Organisation. 16 January 2021. Retrieved 4 June 2021.
- ^ a b "Vaccine shortage attributed to India's expanded coverage for wider population: Experts". The Hindu @businessline. 22 May 2021. Retrieved 4 June 2021.
- ^ a b Jayan, T. V. (3 January 2021). "Covid-19 vaccination: All you need to know". The Hindu @businessline. Retrieved 21 May 2021.
- ^ Pakrasi, Susmita (4 May 2021). "Here's list of states that have declared journalists as frontline workers". Hindustan Times. Retrieved 21 May 2021.
- ^ "Gujarat: Crematorium workers to be considered as frontline warriors". The Economic Times. Press Trust of India. 12 May 2021. Retrieved 21 May 2021.
- ^ Sud, Vedika; Gan, Nectar (19 December 2020). "How India plans to vaccinate 300 million people against Covid-19". CNN. Retrieved 4 June 2021.
- ^ a b c d Sood, Rakesh; Kapur, Kriti; Kurian, Oommen C. (31 May 2021). "India's Vaccine Rollout: A Reality Check". ORF. Retrieved 4 June 2021.
- ^ a b c Sanghi, Neeta (23 April 2021). "The Modi Govt Wants to Vaccinate All Indians. Its Plan Points the Other Way". The Wire Science. Retrieved 4 June 2021.
- ^ Kumar, Parimal (4 April 2021). Achom, Debanish (ed.). "No Fresh Registrations For Healthcare Workers For Covid Vaccine: Centre". NDTV. Retrieved 4 June 2021.
- ^ Dey, Sushmi (19 April 2021). "Only 37% of 3 crore health, frontline workers fully vaccinated". The Times of India. Retrieved 4 June 2021.
- ^ Das, Krishna N. (10 March 2021). "Big Indian state scales down vaccinations, citing shortage". Reuters. Retrieved 4 June 2021.
- ^ Ghosh, Poulomi, ed. (19 March 2021). "'Every vaccine does not require universal immunisation' : Harsh Vardhan on Covid-19 vaccine in Lok Sabha". Hindustan Times. Retrieved 4 June 2021.
- ^ a b Ministry of Health and Family Welfare (19 April 2021). "Government of India announces a Liberalised and Accelerated Phase 3 Strategy of Covid-19 Vaccination from 1st May". PIB. Retrieved 4 June 2021.CS1 maint: uses authors parameter (link)
- ^ RK Dewan & Co (31 May 2021). "NEGVAC clears myths about COVID vaccination in India". Lexology. Retrieved 4 June 2021.CS1 maint: uses authors parameter (link)
- ^ "'Arbitrary and irrational': Supreme Court questions Centre's liberalised vaccination policy". The Financial Express. 2 June 2021. Retrieved 4 June 2021.
- ^ Ellyatt, Holly (5 May 2021). "India is the home of the world's biggest producer of Covid vaccines. But it's facing a major internal shortage". CNBC. Retrieved 4 June 2021.
- ^ "Bangladesh approves China's Sinopharm Covid-19 vaccine for emergency use". Dhaka Tribune. 29 April 2021. Retrieved 4 June 2021.
- ^ Mazumdar, Tulip (17 May 2021). "India's Covid crisis hits Covax vaccine-sharing scheme". BBC News. Retrieved 19 May 2021.
- ^ "Coronavirus: India temporarily halts Oxford-AstraZeneca vaccine exports". BBC News. 24 March 2021. Retrieved 4 June 2021.
- ^ a b Meeting Schedule of the PMO Constituted Vaccine Task Force (VTF) for "Focused Research and Development of Corona Vaccine and other Science and Technology Issues". Office of the Principal Scientific Adviser to the Government of India. 8 May 2021. Retrieved 15 May 2021. Archived on 15 May 2021.
- ^ a b c "National Expert Group on Vaccine Administration for COVID-19 deliberates on strategy to ensure COVID-19 vaccines' availability and its delivery mechanism". pib.gov.in. 12 August 2020. Retrieved 15 May 2021.
- ^ a b c Singh, Nitendra (31 October 2020). "Govt begins preparations for Covid vaccine drive, asks states to set up 3-tier system for rollout". DD News. Retrieved 4 June 2021.
- ^ Dutt, Anonna (8 December 2020). "'300 mn people may get vaccinated simultaneously as per availability of doses': Union health secy". Hindustan Times. Retrieved 4 June 2021.
- ^ "India Preps To Vaccinate 300 Million, Size Of US Population, By July". Agence France-Presse. NDTV. 11 January 2021. Retrieved 4 June 2021.CS1 maint: others (link)
- ^ "Government Launches Mission COVID Suraksha to accelerate Indian COVID-19 Vaccine Development". pib.gov.in. Ministry of Science & Technology. 29 November 2020. Retrieved 5 June 2021.
- ^ Sarda, Kanu (3 June 2021). "Explain how Rs 35,000 crore budget marked for procuring vaccines is being used: SC tells Centre". The New Indian Express. Retrieved 5 June 2021.
- ^ Tarfe, Akshay (3 June 2021). "How India's Covid-19 communication strategy is failing to combat vaccine hesitancy". The Indian Express. Retrieved 4 June 2021.
- ^ Dey, Sushmi (27 May 2021). "Coronavirus vaccine wastage down by half but Chhattisgarh & Jharkhand 'states of concern': Official". The Times of India. Retrieved 5 June 2021.
- ^ "Kerala government announces Rs 20,000 crore package to tackle coronavirus outbreak". Hindustan Times. 20 March 2020. Retrieved 25 March 2020.
- ^ Gaur, Vatsala (21 March 2020). "Yogi Adityanath announces relief measures for UP's daily wage earners". The Economic Times. Retrieved 18 May 2021.
- ^ "Coronavirus: Rs 3,000 relief for construction workers, says Punjab CM Amarinder Singh". The Times of India. TNN. 22 March 2020. Retrieved 22 March 2020.
- ^
- "Karnataka Seals its Borders, Announces Free Ration for All for 2 Months as Covid-19 Cases Reach 20". News18. 22 March 2020. Retrieved 22 March 2020.
- "Bihar CM announces 1 month free supplies for ration card holders". The Times of India. ANI. 23 March 2020. Archived from the original on 10 April 2020. Retrieved 18 February 2021.CS1 maint: others (link)
- "AP announces lockdown till March 31". Outlook India. Press Trust of India. 22 March 2020. Retrieved 18 May 2021.
- "Telangana Lockdown: 12 kg free rice per person ₹1,500 (US$21) per family to be supplied for each white ration card". Telangana Today. 22 March 2020. Retrieved 18 May 2021.
- "COVID-19 causing financial stress to poor, ration per person increased: Arvind Kejriwal". The Economic Times. 21 March 2020. Retrieved 18 May 2021.
- "Over 1 crore people will get free rations: Delhi CM". The Times of India. 22 April 2020. Retrieved 20 May 2021.
- ^ Poovanna, Sharan (6 May 2020). "₹1,610-crore relief for those hardest-hit by lockdown in Karnataka". Livemint. Retrieved 18 May 2021.
- ^ Bhasin, Swati, ed. (14 April 2020). "Rs 1 Crore For Families Of COVID-19 Warriors If They Die: Arvind Kejriwal". NDTV. Retrieved 18 May 2021.
- ^ "Cabinet Meet Live Updates: Centre To Provide 7 Kg Ration To 80 Crore People". BloombergQuint. 25 March 2020. Retrieved 20 May 2021.
- ^ "Coronavirus: FM Sitharaman announces package worth Rs 1,70,000 crore for poor, daily wagers". India Today. 26 March 2020. Archived from the original on 26 March 2020. Retrieved 26 March 2020.
- ^ a b c Ram, Anya Bharat (8 April 2020). "Central government's response to the COVID-19 pandemic (Jan 2020 - Apr 7, 2020)". PRSIndia. Retrieved 21 May 2021.
- ^ "Centre releases Rs 4431 crore to clear pending wages under MGNREGA, to pay all dues by April 10". The Economic Times. 27 March 2020. Retrieved 27 March 2020.
- ^ Iyer, P Vaidyanathan (15 May 2020). "Math behind Rs 20-lakh crore economic package: It is 10% of GDP but about half is already factored in". The Indian Express. Retrieved 15 May 2020.
- ^ "How 10% Of GDP Package Breaks Up: Additional Is Rs 13.5 Lakh Crore". Reuters. NDTV. 13 May 2020. Retrieved 15 May 2020.CS1 maint: others (link)
- ^ Sharma, Manoj (12 November 2020). "Govt announces Atmanirbhar Bharat 3.0; claims COVID stimulus now worth Rs 29.8 lakh crore". Business Today. Retrieved 26 November 2020.
- ^ Ram, Anya Bharat (1 May 2020). "Monthly Policy Review: April 2020. Rs 15,000 crore sanctioned towards the COVID-19 Emergency Response and Health System Preparedness Package". PRS Legislative Research. Retrieved 21 May 2021.
- ^ "COVID-19: Stringency Index". Our World in Data. Retrieved 1 June 2021.
- ^ Hale, Thomas; Angrist, Noam; Goldszmidt, Rafael; Kira, Beatriz; Petherick, Anna; Phillips, Toby; Webster, Samuel; Cameron-Blake, Emily; Hallas, Laura; Majumdar, Saptarshi; Tatlow, Helen (March 2021). "A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker)". Nature Human Behaviour. 5 (4): 529–538. doi:10.1038/s41562-021-01079-8. ISSN 2397-3374. PMID 33686204. S2CID 232160867.
- ^ "India scores high on Covid-19 response tracker made by Oxford University". India Today. 10 April 2020. Retrieved 19 May 2021.
- ^ "Explained: India enforced one of the strongest lockdowns, here's how it stacks up against other countries". The Indian Express. 8 May 2020. Retrieved 26 April 2021.
- ^ Awasthi, Prashasti (12 March 2020). "Centre invokes 'Epidemic Act' and 'Disaster Management Act' to prevent spread of coronavirus". @businessline. Retrieved 19 May 2021.
- ^ Sharma, Ayan (18 March 2020). "How Indian states are gearing up to tackle the coronavirus pandemic". Newslaundry. Retrieved 19 May 2021.
- ^ a b Sanyal, Anindita, ed. (12 March 2020). "India Suspends All Tourist Visas Till April 15 Over Coronavirus: 10 Facts". NDTV. Retrieved 12 March 2020.
- ^
- Bedi, Aneesha (19 March 2020). "Kejriwal govt orders Delhi restaurants to shut shop with immediate effect until 31 March". ThePrint. Retrieved 20 May 2021.
- "All Delhi malls to be closed, grocery and pharmacy stores exempted: CM Arvind Kejriwal". Deccan Herald. Press Trust of India. 20 March 2020. Retrieved 20 March 2020.
- Shukla, Nelanshu (20 March 2020). "Coronavirus outbreak in India: All restaurants, cafes, eateries to remain closed in Lucknow till March 31". India Today. Retrieved 20 May 2021.
- Pinto, Richa (20 March 2020). "Mumbai Lockdown: Many markets and shops in lockdown mode due to Coronavirus". The Times of India. Retrieved 20 May 2021.
- "Coronavirus in Maharashtra: All non-essential shops, offices to shut in Mumbai, Nagpur, Pune". Business Standard. 20 March 2020. Retrieved 20 May 2021.
- "Punjab to enforce lockdown till March 31". The Economic Times. Press Trust of India. 22 March 2020. Retrieved 20 May 2021.
- "Coronavirus: Gehlot orders lockdown in Rajasthan till March 31, exempts essential services". The New Indian Express. 21 March 2020. Retrieved 20 May 2021.
- ^ "PM Modi calls for 'Janata curfew' on March 22 from 7 AM-9 PM". The Hindu @businessline. 20 March 2020. Retrieved 26 April 2021.
- ^ Pandey, Alok (23 March 2020). Bhasin, Swati (ed.). "UP Officials Seen With Crowd Amid "Janata Curfew". Then, A Clarification". NDTV. Retrieved 26 April 2021.
- ^ Regan, Helen; Mitra, Esha; Gupta, Swati (23 March 2020). "India places millions under lockdown to fight coronavirus". CNN. Retrieved 26 April 2021.
- ^ a b "Coronavirus: India enters 'total lockdown' after spike in cases". BBC News. 25 March 2020. Retrieved 26 April 2021.
- ^ "India Covid-19: PM Modi 'did not consult' before lockdown". BBC News. 29 March 2021. Retrieved 26 April 2021.
- ^ Gettleman, Jeffrey; Schultz, Kai (24 March 2020). "Modi Orders 3-Week Total Lockdown for All 1.3 Billion Indians". The New York Times. ISSN 0362-4331. Retrieved 26 April 2021.
- ^ "India coronavirus: All major cities named Covid-19 'red zone' hotspots". BBC. 16 April 2020.
- ^ Bhaskar, Utpal (14 April 2020). "PM Modi announces extension of lockdown till 3 May". Livemint. Retrieved 21 May 2021.
- ^ "India to allow farmers back to work amid lockdown". BBC. 15 April 2020. Retrieved 21 May 2021.
- ^ "2 More Weeks Of Lockdown Starting May 4". NDTV.com. Retrieved 1 May 2020.
- ^ "Coronavirus lockdown extended till 31 May, says NDMA". LiveMint. 17 May 2020. Retrieved 17 May 2020.
- ^ "Lockdown 4.0 guidelines: Centre extends nationwide lockdown till May 31 with considerable relaxations". The Economic Times. 18 May 2020. Retrieved 17 May 2020.
- ^ Sharma, Neeta (30 May 2020). Ghosh, Deepshikha (ed.). ""Unlock1": Malls, Restaurants, Places Of Worship To Reopen June 8". NDTV. Retrieved 30 May 2020.
- ^ "Ministry of Home Affairs Unlock 5.0 official guidelines on their official website" (PDF). Ministry of Home Affairs.
- ^ "Unlock 6.0 latest guidelines: What do they mean for schools, colleges, other educational institutions". DNA India. 29 October 2020. Retrieved 11 November 2020.
- ^ a b Ghosh, Jayati (11 July 2020). "A critique of the Indian government's response to the COVID-19 pandemic". Journal of Industrial and Business Economics. 47 (3): 519–530. doi:10.1007/s40812-020-00170-x. ISSN 0391-2078. PMC 7351648.
- ^ Singh, Sunilkumar (23 February 2021). Dey, Stela (ed.). ""Please Cooperate, Else...": Cops On Lockdown In Maharashtra's Amravati". NDTV. Retrieved 1 June 2021.
- ^ Upadhyay, Pankaj (15 March 2021). "Nagpur imposes 7-day lockdown from today as coronavirus cases continue to rise in Maharashtra". India Today. Retrieved 1 June 2021.
- ^ Gupta, Saurabh (5 April 2021). Roy, Divyanshu Dutta (ed.). "Weekend Lockdown In Maharashtra, 8 PM-7 AM Curfew Amid Covid Surge". NDTV. Retrieved 1 June 2021.
- ^ a b "Covid-19 second wave: Here's a list of states that have imposed full lockdown". The Indian Express. 9 May 2021. Retrieved 19 May 2021.
- ^ a b Sangal, Aditi (17 May 2021). "Analysis: Another national lockdown is not realistic for India". CNN. Retrieved 19 May 2021.
- ^ Ail, Arundhati (31 May 2021). "All the new lockdown guidelines across India in June". Condé Nast Traveller India. Retrieved 1 June 2021.
- ^ Code of Practice. National Technical Advisory Group on Immunisation. Ministry of Health and Family Welfare. July 2015. p 3. Retrieved 22 May 2021. "As India’s apex advisory body on immunization, the NTAGI provides guidance and advice to the MoHFW [...]"
- ^ a b c Ghosh, Abantika (17 May 2021). "Too many cooks? 15 committees, dozens of experts behind India's fumbling Covid response". ThePrint. Retrieved 22 May 2021.
- ^ "India's Policy Response to COVID-19" (PDF). The Center for Policy Impact in Global Health. June 2020. Retrieved 23 May 2021.
- ^ "Health Ministry reviews preparedness for Novel Corona Virus(nCoV)". Press Information Bureau, Government of India. Ministry of Health and Family Welfare. 17 January 2020. Retrieved 23 May 2021.CS1 maint: others (link)
- ^ a b "ICMR sets up national task force on Covid-19, will also decide on lockdown". Hindustan Times. 7 April 2020. Retrieved 15 May 2021.
- ^ "High-level Group of Ministers reviews preparedness to tackle coronavirus". Business Today. 13 February 2020. Retrieved 20 May 2021.
- ^ "Dr Harsh Vardhan chairs 26th meeting of Group of Ministers (GOM) on COVID-19". Press Information Bureau, Government of India. Ministry of Health and Family Welfare. 17 May 2021. Retrieved 20 May 2021.CS1 maint: others (link)
- ^ Gupta, Moushumi Das; Dhingra, Sanya (29 March 2020). "PM Modi sets up 11 empowered groups as quick response teams to tackle coronavirus outbreak". ThePrint. Retrieved 15 May 2021.
- ^ "Two institutes in Bengaluru to lead India's Covid prediction model". The Times of India. 31 May 2020. Retrieved 15 May 2021.
- ^ "National Expert Group on Vaccine Administration for COVID19". JournalsOfIndia. 15 January 2021. Retrieved 15 May 2021.
- ^ Ghosh, Abantika (14 September 2020). "Modi govt's 11 Covid empowered panels now replaced by six larger groups". ThePrint. Retrieved 15 May 2021.
- ^ "Coronavirus | MHA reconstitutes empowered groups". The Hindu. PTI. 2 May 2020. ISSN 0971-751X. Retrieved 15 May 2021.CS1 maint: others (link)
- ^ "Coronavirus: Empowered group likely to firm up medical emergency plan in next few days". The Indian Express. 31 March 2020. Retrieved 15 May 2021.
- ^ Sharma, Milan (30 October 2020). "Centre directs states to form committees to oversee Covid-19 vaccination drive". India Today. Retrieved 4 June 2021.
- ^ "Centre Asks States To Form Committees For Smooth COVID-19 Vaccination Drive". Press Trust of India. NDTV. 30 October 2020. Retrieved 4 June 2021.CS1 maint: others (link)
- ^ "Genome Sequencing by INSACOG shows variants of concern and a Novel variant in India". Press Information Bureau, Government of India. Ministry of Health and Family Welfare. 24 March 2021. Retrieved 20 May 2021.CS1 maint: others (link)
- ^ "Indian SARS-CoV-2 Genomic Consortia (INSACOG) launched,coordinated by Department of Biotechnology (DBT) along with MoH&FW, ICMR, and CSIR | Department of Biotechnology". Department of Biotechnology, Ministry of Science and Technology, Government of India. Press Information Bureau. 30 December 2020. Retrieved 20 May 2021.CS1 maint: others (link)
- ^ G, Ananthakrishnan (9 May 2021). "SC sets up task force for Covid response, oxygen audit, supply". The Indian Express. Retrieved 15 May 2021.
- ^ "Health ministry releases communication strategy to support Covid-19 vaccine rollout | India News - Times of India". The Times of India. PTI. 31 December 2020. Retrieved 4 June 2021.CS1 maint: others (link)
- ^ a b c d ANI (1 May 2021). "This is a war, we need to win, says Lt General Madhuri Kanitkar on Covid". Business Standard India. Retrieved 10 May 2021.
- ^ "Indian Army operationalises dedicated COVID facility in Pune". ANI News. 29 April 2021. Retrieved 10 May 2021.
- ^ "DRDO, Gujarat govt set up 900-bed Covid-19 hospital in Ahmedabad". mint. PTI. 25 April 2021. Retrieved 10 May 2021.CS1 maint: others (link)
- ^ a b c "Raksha Mantri Shri Rajnath Singh reviews efforts of MoD & Armed Forces in fight against second COVID-19 wave;". pib.gov.in. 1 May 2021. Retrieved 10 May 2021.
- ^ Prabhu, Sunil (26 April 2021). "Retired Military Medics Recalled To Work At Covid Facilities". NDTV. Retrieved 10 May 2021.
- ^ "PM Modi reviews Army's preparedness, initiatives for management of spiralling Covid-19 crisis". Hindustan Times. 29 April 2021. Retrieved 10 May 2021.
- ^ "Operation CO-JEET launched by armed forces to fight COVID-19 in India: Lt Gen Kanitkar". The Economic Times. PTI. 3 May 2021. Retrieved 12 June 2021.
- ^ Bajwa, Mandeep Singh (19 July 2020). "Military Digest | Detailed Order of Battle: Chinese Forces in Eastern Ladakh". The Indian Express. Retrieved 12 June 2021.
- ^ Bhalla, Abhishek (2 May 2021). "Indian Navy launches operation Samudra Setu-II to bring medical oxygen from abroad". India Today. Retrieved 12 June 2021.
- ^ "Coronavirus outbreak: Vivo to donate 1 lakh protective masks to Maharashtra Govt, Xiaomi suspends local manufacturing". The Financial Express.
- ^ "Coronavirus Lockdown: Hyundai India Orders Advanced COVID-19 Testing Kits From Korea". CarandBike. Retrieved 28 March 2020.
- ^ "IIT Hyderabad provides 100 litres of hand-sanitiser everyday to combat Covid-19". The Times of India. Retrieved 17 April 2020.
- ^ "Tata Sons' Rs 1,000 cr top-up takes group coronavirus fund to Rs 1,500 cr – India's biggest". Business Today. Retrieved 2 April 2020.
- ^ "Azim Premji's foundation, Wipro commit Rs 1,125 crore as India battles with coronavirus". The Financial Express. Retrieved 2 April 2020.
- ^ "Coronavirus Outbreak: Reliance Industries announces Rs 500 crore contribution to PM-CARES fund". Firstpost. Retrieved 2 April 2020.
- ^ "Covid-19: Aditya Birla Group donates Rs 500 crores in PM-CARES fund". India Today. Retrieved 13 April 2020.
- ^ Pathak, Kalpana; Tandon, Suneera (27 April 2021). "India Inc steps up effort to fight pandemic". mint. Retrieved 10 May 2021.
- ^ Kumari, Honey (10 May 2021). "How Global & Domestic Industries Lent a Helping Hand". Silicon India. Retrieved 10 May 2021.
- ^ "From Amazon to Tata, Reliance to Vedanta, industry steps up to combat COVID". mint. 9 May 2021. Retrieved 10 May 2021.
- ^ "CEOs of 40 US companies create global task force to help India fight COVID-19". mint. 27 April 2021. Retrieved 10 May 2021.
- ^ "Ola to start doorstep delivery of oxygen concentrators to consumers". The Indian Express. 10 May 2021. Retrieved 10 May 2021.
- ^ "Vaccine Supply (Made-in-India COVID19 vaccine supplies so far)". Ministry of External Affairs – Government of India. 20 May 2021. Archived from the original on 21 May 2021. Retrieved 21 May 2021.
- ^ a b "United States Airlifts Emergency Supplies to Help India Address Deadly Second Wave of COVID-19 Pandemic | Press Release". U.S. Agency for International Development (USAID). 7 May 2021. Retrieved 10 May 2021.
- ^ Laskar, Rezaul H (29 April 2021). "'Over 40 countries to help India in fight against Covid-19': Harsh Shringla". Hindustan Times. Retrieved 10 May 2021.
- ^ "Coronavirus: EU channels critical support to India via EU Civil Protection Mechanism". European Commission. 27 April 2021. Retrieved 10 May 2021.
- ^ Basu, Nayanima (4 May 2021). "Germany sending 'massive' oxygen plant, 12 army paramedics to operate it, envoy Lindner says". ThePrint. Retrieved 10 May 2021.
- ^ "Delhi Gets 3 Out Of 21 Oxygen Plants From France". PTI. NDTV. 9 May 2021. Retrieved 10 May 2021.CS1 maint: others (link)
- ^ "IAF conducts 160 sorties to facilitate oxygen supply across India". The Times of India. 30 April 2021. Retrieved 10 May 2021.
- ^ Quito, Anne (25 April 2021). "The world is starting to grasp the true toll of India's Covid-19 crisis". Quartz. Retrieved 10 May 2021.
- ^ "Russia sends 22 tonnes of Covid relief material to help India fight Covid-19". The Indian Express. 29 April 2021. Retrieved 10 May 2021.
- ^ "UNICEF sends 3,000 oxygen concentrators and other critical supplies to India as country battles deadly COVID-19 surge". unicef.org. 29 April 2021. Retrieved 10 May 2021.
- ^ Madjar, Kayleigh (30 April 2021). "Nation sends oxygen machines to India". Taipei Times. Retrieved 2 May 2021.
- ^ PTI (27 April 2021). "Bhutan to supply liquid oxygen to India to help combat Covid crisis". ThePrint. Retrieved 10 May 2021.
- ^ Bhattacherjee, Kallol (6 May 2021). "Coronavirus | Bangladesh gifts India 10,000 Remdesivir vials". The Hindu. ISSN 0971-751X. Retrieved 10 May 2021.
- ^ "Kuwait sends emergency supplies of liquid oxygen to India as COVID-19 cases surge". Arab News. 17 May 2021. Retrieved 20 May 2021.
- ^ "Kenya Covid-19 relief India: Kenya donates 12 tonnes of food products to India". The Times of India. PTI. 30 May 2021. Retrieved 1 June 2021.CS1 maint: others (link)
- ^ "India received 2,060 oxygen concentrators, three oxygen generation plants as foreign aid". The Hindu. PTI. 8 May 2021. ISSN 0971-751X. Retrieved 10 May 2021.CS1 maint: others (link)
- ^ "'COVID-19 shared problem; what you call aid, we call friendship': EAM S Jaishankar". businesstoday.in. 5 May 2021. Retrieved 10 May 2021.
- ^ Chaudhury, Dipanjan Roy (16 April 2020). "China dispatches 650,000 medical kits to India to fight COVID-19: Indian envoy". The Economic Times. Retrieved 16 April 2020.
- ^ Hunter, Jack (6 May 2021). "India Covid aid: Is emergency relief reaching those in need?". BBC News. Retrieved 5 June 2021.
- ^ "Department Press Briefing - April 30, 2021". United States Department of State. Retrieved 5 June 2021.
We are sending these planeloads of material to India. But our journalist in Delhi is reporting that even after trying for two days he’s been unable to find out who is taking away the oxygen concentration, medicines, or how much is arriving. There’s no website or transparent system where people can apply to get this. So this accountability for the U.S. taxpayers’ money being sent, is there anything being done to check on how it is being distributed, the aid that we are sending?
- ^ a b "India got over 57 lakh foreign aid items till May 4 but 3 lakh items not sent out till May 6: Report". Scroll.in. 14 May 2021. Retrieved 5 June 2021.
- ^ "COVID Relief: Here is the full list of foreign aid dispatched to states/UTs". mint. 14 May 2021. Retrieved 5 June 2021.
- ^ "How foreign aid to fight COVID-19 in India is being allocated to different states. Equitable distribution to states". The Economic Times. 5 May 2021. Retrieved 5 June 2021.
- ^ Chatterji, Saubhadra (9 May 2021). "Delhi given large part of foreign aid: Data". Hindustan Times. Retrieved 5 June 2021.
- ^ a b Krishnan, Vidya (12 May 2020). "Epidemiologists say India's centre for disease control withheld COVID-19 data since pandemic began". The Caravan. Retrieved 23 May 2021.
- ^ a b Bhatia, Surbhi; Alexander, Sneha (29 March 2020). "Covid-19 shows why we need a healthcare reboot for India". mint. Retrieved 23 May 2021.
- ^ Krishnan, Murali (26 April 2021). "Coronavirus: Is India counting all COVID deaths?". DW. Retrieved 23 May 2021.
- ^ Chatterjee, Patralekha (5 September 2020). "Is India missing COVID-19 deaths?". The Lancet. 396 (10252): 657. doi:10.1016/S0140-6736(20)31857-2. ISSN 0140-6736. PMC 7470692. PMID 32891197.
- ^ Bhardwaj, Deeksha (10 April 2020). "Covid-19 crisis: States asked to fill 227 vacancies for epidemiologists". Hindustan Times. Retrieved 23 May 2021.
- ^ Varshney, Vibha (24 July 2021). "India's mysterious diseases: What is NCDC doing?". Down to Earth. Retrieved 23 May 2021.
- ^ a b Krishnan, Vidya (22 April 2021). "India's COVID-19 taskforce did not meet in February, March despite surge, say members". The Caravan. Retrieved 20 May 2021.
Another significant lapse, the members told me, the Indian Council of Medical Research’s failure to update the treatment protocol for COVID-19 in the past nine months, since July 2020.
- ^ Rampal, Nikhil (12 May 2021). "Why India's second wave has been deadlier, explained in five charts". mint. Retrieved 23 May 2021.
- ^ Menon, Gautam I. (24 October 2020). "Problems with the Indian supermodel for COVID-19". The Hindu. ISSN 0971-751X. Retrieved 20 May 2021.
- ^ IANS (4 May 2021). "Couldn't predict exact nature of second Covid wave: Supermodel Committee". Business Standard India. Retrieved 20 May 2021.
- ^ Banaji, Murad (14 May 2021). "Flawed science propped up India's second COVID-19 wave". The Caravan. Retrieved 20 May 2021.
- ^ M, Kaunain Sheriff (5 May 2021). "Third Covid wave inevitable, didn't foresee current ferocity: Scientific Advisor to PM". The Indian Express. Retrieved 23 May 2021.
- ^ Prabhu, Sunil (5 May 2021). Roy, Divyanshu Dutta (ed.). "Third Wave Inevitable, Says Centre: 10 Facts On Centre's Covid Update". NDTV. Retrieved 23 May 2021.
- ^ Roy, Divyanshu Dutta, ed. (7 May 2021). "If We Take Strong Measures, Third Wave Of COVID-19 May Not Happen: Government". NDTV. Retrieved 23 May 2021.
- ^ Chaudhury, Dipanjan Roy; Pubby, Manu (27 April 2021). "Lab origin not ruled out as India studying all aspects of Covid-19". The Economic Times. Retrieved 29 May 2021.
- ^ Gupta, Shishir (17 May 2020). "Eye on China, India backs 62-nation coalition's push for probe into Covid-19 origin". Hindustan Times. Retrieved 29 May 2021.
- ^ "In research preprint, Chinese scientists claim COVID-19 may have originated in India or Bangladesh-Health News , Firstpost". Firstpost. 29 November 2020. Retrieved 29 May 2021.
- ^ "India for more studies to trace Covid origin". The Times of India. 29 May 2021. Retrieved 29 May 2021.
- ^ "'Important first step': India backs WHO study on Covid-19 origins". Hindustan Times. ANI. 29 May 2021. Retrieved 29 May 2021.CS1 maint: others (link)
- ^ Biswas, Soutik (30 March 2020). "Coronavirus: India's pandemic lockdown turns into a human tragedy". BBC News. Retrieved 14 May 2021.
- ^ Sanghera, Tish (2 April 2020). "Hungry, desperate: India virus controls trap its migrant workers". Al Jazeera. Retrieved 14 May 2021.
- ^ Slater, Joanna; Masih, Niha (28 March 2020). "In India, the world's biggest lockdown has forced migrants to walk hundreds of miles home". The Washington Post. Retrieved 13 May 2020.
- ^ Borbon, Christian (28 March 2020). "Indian migrants forced to walk home amid COVID-19 lockdown". Gulf News. Retrieved 13 May 2020.
- ^ Ara, Ismat (29 March 2020). "'No Work, No Money': Thousands Stranded on Anand Vihar Bus Stand". The Wire. Retrieved 14 May 2021.
- ^ "More than 21,000 camps set up for over 6,60,000 migrants: State governments". The Economic Times. 1 April 2020. Retrieved 2 April 2020.
- ^ "Coronavirus lockdown | Over 60,000 people have registered on Delhi govt portal to go back home". The Hindu. Press Trust of India. 15 May 2020. ISSN 0971-751X. Retrieved 18 May 2020.
- ^ Jha, Somesh (29 March 2020). "Fighting Covid-19: After the long walk, jobless migrants head home by bus". Business Standard India. Retrieved 14 May 2021.
- ^ Pandey, Devesh K. (29 March 2020). "Coronavirus | Migrant workers to be stopped, quarantined at borders, says Centre". The Hindu. ISSN 0971-751X. Retrieved 2 May 2020.
- ^ Dubey, Vivek (29 March 2020). "Coronavirus crisis: Landlords can't ask rent from students, workers for 1 month". Business Today. Retrieved 14 May 2021.
- ^ Chaturvedi, Arpan (1 April 2020). "Government Effort To Restrain Media Coverage Of Pandemic Met With Supreme Court Caution". BloombergQuint. Retrieved 10 May 2020.
- ^ Rajalakshmi, T. K. (1 April 2020). "Centre blames media 'fake news' for mass migration during lockdown". The Hindu Frontline. Retrieved 10 May 2020.
- ^ Bhargava, Yuthika (1 May 2020). "Coronavirus lockdown | Railways to run 'Shramik Special' trains to move migrant workers, other stranded persons". The Hindu. ISSN 0971-751X. Retrieved 9 May 2020.
- ^ "Shramik special trains | Migrant workers, other stranded people to pay ₹50 more to get home". The Hindu. 2 May 2020. ISSN 0971-751X. Retrieved 9 May 2020.
- ^ Anuja; Varma, Gyan (4 May 2020). "Congress' move to sponsor rail fare for migrants sparks political tussle". Livemint. Retrieved 9 May 2020.
- ^ "Government can't tell Supreme Court if it is paying 85% rail fare". The Telegraph. Kolkota. 6 May 2020. Retrieved 23 May 2020.
- ^ Rajagopal, Krishnadas (26 May 2020). "Supreme Court orders Centre and States to immediately provide transport, food and shelter free of cost to stranded migrant workers". The Hindu. ISSN 0971-751X. Retrieved 27 May 2020.
- ^ Chandna, Himani (30 January 2020). "India's production of paracetamol, top antibiotics could be hit by China coronavirus crisis". ThePrint. Retrieved 11 May 2021.
- ^ a b Ellis-Petersen, Hannah (4 March 2020). "India limits medicine exports after supplies hit by coronavirus". The Guardian. Retrieved 11 May 2021.
- ^ Pandey, Vikas (15 April 2021). "India coronavirus: Desperate Covid-19 patients turn to black market for drugs". BBC News. Retrieved 17 April 2021.
- ^ "India's Covid-19 shortages spur black market for drugs, oxygen". AFP. France 24. 22 April 2021. Retrieved 11 May 2021.CS1 maint: others (link)
- ^ "U.S. drugmakers step up supplies as India battles COVID-19 surge". Reuters. 26 April 2021. Retrieved 11 May 2021.
- ^ Leo, Leroy (20 April 2021). "Vitamins, antivirals shortage piles woes on covid patients". mint. Retrieved 11 May 2021.
- ^ Chandna, Himani (3 May 2021). "Pharma industry warns of Covid drug shortages as raw materials prices surge 200%". ThePrint. Retrieved 11 May 2021.
- ^ Sanyal, Anindita, ed. (17 March 2020). "Schools Closed, Travel To Be Avoided, Says Centre On Coronavirus: 10 Points". NDTV. Retrieved 18 March 2020.
- ^ Iftikhar, Fareeha; Sarfaraz, Kainat (18 March 2020). "CBSE Board advises social distancing, face masks at exam centres to prevent coronavirus". Hindustan Times. Retrieved 14 May 2021.
- ^ "CBSE 10th and 12th Board exams postponed due to coronavirus epidemic". The Times of India. 19 March 2020. Retrieved 15 May 2021.
- ^ "MP Board 10th & 12th exams postponed due to Coronavirus". The Times of India. 20 March 2020. Retrieved 14 May 2021.
- ^ M.K., Nidheesh (20 March 2020). "COVID-19: Kerala postpones Class 10, Class 12 board exams, a first for the state". Livemint. Retrieved 14 May 2021.
- ^ Tandon, Tulika (20 March 2020). "Assam Government cancels all exams till March 31 due to COVID19, new dates to be out soon". Times Now News. Retrieved 14 May 2021.
- ^ "Coronavirus outbreak: UPSC defers civil services interviews". The Economic Times. 20 March 2020. Retrieved 14 May 2021.
- ^ Modi, Sushma; Postaria, Ronika (6 October 2020). "How COVID-19 deepens the digital education divide in India". UNICEF Global Development Commons. Retrieved 12 May 2021.
- ^ Nanda, Prashant K. (28 October 2020). "Digital divide is stark, online education still far from reality: ASER". mint. Retrieved 12 May 2021.
- ^ Kundu, Protiva (5 May 2020). "Indian education can't go online – only 8% of homes with young members have computer with net link". Scroll.in. Retrieved 12 May 2021.
- ^ Dugal, Ira (3 May 2021). "Covid Second Wave: Economic Impact Not Trivial But May Be Less Enduring, Say Economists". BloombergQuint. Retrieved 12 May 2021.
- ^ "Impact Of COVID-19 Second Wave On Economy To Remain Muted: Finmin Report". BW Businessworld. 7 May 2021. Retrieved 12 May 2021.
- ^ "'Covid wave: Expect muted hit on economy as against first'". The Indian Express. 8 May 2021. Retrieved 12 May 2021.
- ^ "Editorial: The economic impact of Covid-19". Hindustan Times. 6 May 2021. Retrieved 12 May 2021.
- ^ "Sensex witnesses flash crash on 2 new coronavirus cases in India; over 340 stocks hit 52-week low". Moneycontrol. Retrieved 3 March 2020.
- ^ "Sensex Crashes 2,919 Points, Nifty Ends at 9,590 In Worst Day For Markets Ever". NDTV.com. Retrieved 13 March 2020.
- ^ "Stock markets post worst losses in history; Sensex crashes 3,935 points amid coronavirus lockdown". The Indian Express. 23 March 2020. Retrieved 23 March 2020.
- ^ "Sensex crashes 4,000 points: What's behind market meltdown". The Economic Times. 23 March 2020. Retrieved 23 March 2020.
- ^ Shah, Ami (25 March 2020). "Sensex posts biggest gain in 11 years: Investors richer by Rs 4.7 lakh crore". The Economic Times. Retrieved 25 March 2020.
- ^ Das, Shouvik (25 March 2020). "Flipkart to Resume Shipping and Deliveries from Later Today, Confirms CEO". News18. Retrieved 25 March 2020.
- ^ Singh, Sandeep (6 May 2021). "Explained: Why markets are rising despite Covid-19 surge, what you should do". The Indian Express. Retrieved 12 May 2021.
- ^ Lyons, Kim (24 April 2021). "Twitter censored tweets critical of India's handling of the pandemic at its government's request". The Verge. Retrieved 24 April 2021.
- ^ Deep, Aroon (24 April 2021). "Twitter censors tweets from MP, MLA, editor criticising pandemic handling". MediaNama. Retrieved 24 April 2021.
- ^ Singh, Karan Deep; Mozur, Paul (25 April 2021). "As Outbreak Rages, India Orders Critical Social Media Posts to Be Taken Down". The New York Times. ISSN 0362-4331. Retrieved 26 April 2021.
- ^ "No clampdown on grievances; must avoid political bickering: What SC said on Covid crisis". The Times of India. 30 April 2021. Retrieved 11 May 2021.
- ^ "Covid: India tells social media firms to remove 'India variant' from content". BBC News. 22 May 2021. Retrieved 22 May 2021.
- ^ "India TB Report 2021: National Tuberculosis Elimination Programme. Annual Report". Central TB Division. Ministry of Health and Family Welfare. Government of India. p. 12. Retrieved 21 May 2021.
- ^ a b Roberts, Leslie (21 April 2021). "How COVID hurt the fight against other dangerous diseases". Nature. 592 (7855): 502–504. doi:10.1038/d41586-021-01022-x. PMID 33883727. S2CID 233349507.
- ^ Mascarenhas, Anuradha (19 March 2021). "One year of Covid-19 eliminated 12 years of progress in global fight against tuberculosis". The Indian Express. Retrieved 21 May 2021.
- ^ Sharma, Neetu Chandra (25 March 2021). "India tuberculosis registrations fall 24% in 2020 due covid-led disruptions". mint. Retrieved 21 May 2021.
- ^ "IMA says nearly 200 doctors in India have succumbed to COVID-19 so far; requests PM's attention". The Economic Times. 8 August 2020. Retrieved 9 August 2020.
- ^ "IMA Says At Least 515 Doctors Have Died of COVID-19". The Wire Science. 2 October 2020. Retrieved 13 February 2021.
- ^ "IMA publishes list of 382 doctors who died due to Covid-19, demands they be treated as martyrs". Hindustan Times. PTI. 16 September 2020. Retrieved 13 February 2021.CS1 maint: others (link)
- ^ a b "IMA refutes govts data, says 734 doctors died due to Covid-19, condemns Centres apathy". Hindustan Times. ANI. 3 February 2021. Retrieved 13 February 2021.CS1 maint: others (link)
- ^ a b "174 Doctors, 116 Nurses, 199 Health Workers Died Due To Covid: Centre". PTI. NDTV. 5 February 2021. Retrieved 11 May 2021.CS1 maint: others (link)
- ^ a b Mascarenhas, Anuradha (17 April 2021). "747 doctors died of Covid-19 in India: IMA". The Indian Express. Retrieved 11 May 2021.
- ^ Dey, Sushmi (29 August 2020). "87k health staff infected with Covid, 573 dead; 74% cases from six states". The Times of India. Retrieved 11 May 2021.
- ^ Roy, Divyanshu Dutta, ed. (16 January 2021). ""Humbled And Proud": Frontline Workers On Getting First Covid Vaccines". NDTV. Retrieved 14 May 2021.
- ^ Sinha, Smriti, ed. (14 May 2021). "India has administered nearly 180mn Covid vaccine doses till now". Hindustan Times. Retrieved 14 May 2021.
- ^ Bhasin, Swati, ed. (4 March 2020). "Why PM Modi Won't Participate In Holi Events This Year". NDTV. Retrieved 11 May 2021.
- ^ Kumar, Rakesh (21 September 2020). "Covid-19 is changing how India marks its religious festivals". South China Morning Post. Retrieved 11 May 2021.
- ^ "Even as Uttarakhand Reels From Sharp Spike in COVID Cases, Char Dham Yatra To Go Ahead". The Wire. 28 April 2021. Retrieved 11 May 2021.
- ^ Upadhyay, Vineet (23 July 2020). "Char Dham Yatra: Uttarakhand mulling to allow pilgrims from other states". The New Indian Express. Retrieved 11 May 2021.
- ^ Menon, Shailesh (2 April 2020). "God goes online as places of worship shut doors to save people". The Economic Times. Retrieved 6 June 2020.
- ^ Sharad, Arpita (23 March 2020). "Followers catch up on church service streaming live on various platforms". The Times of India. Retrieved 30 March 2020.
- ^ SOP on preventive measures to contain spread of COVID-19 in religious places/places of worship (PDF) (Report). Ministry of Health and Family Welfare. 4 June 2020. Retrieved 6 June 2020.
- ^ Slater, Joanna; Masih, Niha; Irfan, Shams (2 April 2020). "India confronts its first coronavirus 'super-spreader' – a Muslim missionary group with more than 400 members infected". The Washington Post.
- ^ "Kumbh Mela was super-spreader event in India: Report". The Week. 10 May 2021. Retrieved 11 May 2021.
- ^ Upadhyay, Vineet (27 April 2021). "Mahakumbh impact? Uttarakhand active Covid caseload jumped 1,800% in 25 days". The New Indian Express. Retrieved 11 May 2021.
- ^ "After Kumbh, Uttarakhand Sees 1800% Jump in COVID-19 Cases". TheQuint. 8 May 2021. Retrieved 11 May 2021.
- ^ "Despite surge in cases, Covid guidelines flouted during Holi celebrations". The Indian Express. 29 March 2021. Retrieved 11 May 2021.
- ^ Sadam, Rishika (8 May 2021). "Covid protocols up in the air in Hyderabad's Eid markets, vendors say need to earnCovid protocols up in the air in Hyderabad's Eid markets, vendors say need to earn". ThePrint. Retrieved 11 May 2021.
- ^ "Census of India: Rural-Urban Distribution". censusindia.gov.in. Office of the Registrar General & Census Commissioner, India, Ministry of Home Affairs, Government of India. Archived from the original on 25 February 2021. Retrieved 15 May 2021.
- ^ a b c Acharjee, Sonali (21 September 2020). "The rural surge". India Today. Retrieved 15 May 2021.
- ^ Singh, Karan Deep; Gettleman, Jeffrey (8 October 2020). "'Rural Surge' Propels India Toward More Covid-19 Infections Than U.S." The New York Times. ISSN 0362-4331. Retrieved 15 May 2021.
- ^ Chauhan, Chetan (14 May 2021). "As Covid second wave persists, MGNREGS comes to rural India's rescue, yet again". Hindustan Times. Retrieved 15 May 2021.
- ^ "More than 4,000 Indians die of COVID for second straight day". Al Jazeera. 13 May 2021. Retrieved 15 May 2021.
- ^ Noronha, Rahul (1 May 2021). "Ground report: How Covid-19 has affected India's rural areas". India Today. Retrieved 15 May 2021.
- ^ Das, Krishna (15 May 2021). "Bodies of COVID-19 victims among those dumped in India's Ganges -govt document". Reuters. Retrieved 16 May 2021.
- ^ "IndiGo cancels flights on Delhi-Istanbul, Chennai-Kuala Lumpur route from March18–31". Business Standard. Press Trust of India. 17 March 2020. Retrieved 20 March 2020.
- ^ Kundu, Rhik (17 March 2020). "GoAir suspends international operations". mint. Retrieved 18 March 2020.
- ^ "No international commercial flight will be allowed to land India from March 22". IndiaTV. 19 March 2020. Retrieved 14 May 2021.
- ^ Kundu, Rhik (23 March 2020). "Coronavirus: India suspends domestic flights from 25 March". Livemint. Retrieved 14 May 2021.
- ^ Majumder, Arindam; Phadnis, Aneesh (5 May 2020). "India set to bring home 250,000 stranded abroad; 64 flights deployed". Business Standard India. Retrieved 10 May 2021.
- ^ "Air India Express plane skids off runway, killing at least 18 and injuring more than 100". CBS News. Associated Press. 7 August 2020. Retrieved 10 August 2020.
- ^ "Kozhikode Air India Express crash: CISF personnel quarantined after passengers test positive for coronavirus". The Indian Express. 8 August 2020. Retrieved 8 August 2020.
- ^ "Coronavirus: Central, Western Railway withdraw curtains, blankets from AC coaches". Business Standard India. Press Trust of India. 14 March 2020. Retrieved 14 May 2021.
- ^ Sharma, Anu (17 March 2020). "Coronavirus impact: Railway platform ticket price hiked to Rs 50 in 250 stations". CNBC TV18. Retrieved 14 May 2021.
- ^ Dash, Dipak K (21 March 2020). "Janata curfew: 3,700 trains cancelled on Sunday". The Times of India. Retrieved 14 May 2021.
- ^ "Metro services shut across India till March 31". The Economic Times. Press Trust of India. 22 March 2020. Retrieved 22 March 2020.
- ^ "After trains, interstate bus services suspended till 31st March". The Economic Times. 22 March 2020. Retrieved 14 May 2021.
- ^ "IRCTC suspends bookings for its 3 private trains till April 30, amid nationwide lockdown due to coronavirus COVID-19". sarkaripaper.co,in. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- ^ Agarwal, Nikhil (14 April 2020). "Train services suspended till May 3, no ticket booking till further orders". Livemint. Retrieved 16 April 2020.
- ^ "Aurangabad train accident: 16 migrant workers run over, probe ordered". The Indian Express. 8 May 2020. Retrieved 18 February 2021.
- ^ "Bus services between Indore and Maharashtra to be suspended". India Today. PTI. 18 March 2020. Retrieved 14 May 2021.CS1 maint: others (link)
- ^ Vasdev, Kanchan (20 March 2020). "Punjab to ban public transport from March 21". The Indian Express. Retrieved 19 March 2020.
- ^ "Govt bans public transport in Srinagar to prevent spread of Coronavirus". Greater Kashmir. 19 March 2020. Retrieved 19 March 2020.
- ^ Nanisetti, Serish (22 March 2020). "Panicky shoppers clear out grocery shops". The Hindu. Retrieved 22 March 2020.
- ^ "No need for panic buying of milk". Ahmedabad Mirror. 22 March 2020. Retrieved 22 March 2020.
- ^ Malviya, Sagar; Bhushan, Ratna (20 March 2020). "Panic buying goes a notch up ahead of PM Modi's address". The Economic Times. Retrieved 14 May 2021.
- ^ "Janata curfew, avoid panic buying, stay at home: PM Modi's 9 key messages for Indians". The Times of India. 19 March 2020. Retrieved 15 May 2021.
- ^ Biswas, Soutik (7 April 2020). "Will coronavirus lockdown cause food shortages in India?". BBC News. Retrieved 14 May 2021.
- ^ Yadav, Anumeha (19 April 2020). "India: Hunger and uncertainty under Delhi's coronavirus lockdown". Al Jazeera. Retrieved 14 May 2021.
- ^ Roy, Rajesh; Agarwal, Vibhuti (8 April 2020). "India's Food Supply Chain Frays as People Stay Home". The Wall Street Journal. Retrieved 14 May 2021.
- ^ "Coronavirus: India Open Badminton Tournament Cancelled". Outlook. Press Trust of India. 14 March 2020. Retrieved 14 March 2020.
- ^ Mukherjee, Soham (14 March 2020). "Coronavirus: I-League matches suspended from March 15". Goal.com. Retrieved 18 March 2020.
- ^ Mergulhao, Marcus (13 March 2020). "Coronavirus: ISL final to be held behind closed doors". The Times of India. Retrieved 13 March 2020.
- ^ "Refund process for Hero ISL 2019–20 final ticket holders". Indian Super League. 12 March 2021. Retrieved 13 March 2020.
- ^ Biji Babu Cyriac (26 March 2020). "TCS World 10K Bengaluru postponed". The Times of India. Retrieved 5 April 2020.
- ^ "India's FIFA World Cup qualifier against Qatar postponed due to coronavirus outbreak". India Today. Archived from the original on 8 March 2020. Retrieved 7 March 2020.
- ^ "Virus hits Indian sports". The Economic Times. Press Trust of India. 6 March 2020. Retrieved 7 March 2020.
- ^ Gollapudi, Nagraj (14 April 2020). "With India in lockdown, IPL 2020 suspended indefinitely". ESPNcricinfo. Retrieved 15 April 2020.
- ^ Rao, K Shriniwas (13 March 2020). "It's official: IPL 2020 postponed to April 15 due to coronavirus". The Times of India. Retrieved 13 March 2020.
- ^ "Indian government gives IPL 2020 the green signal". ESPNcricinfo. 2 August 2020. Retrieved 2 August 2020.
- ^ Rao, Rakesh (13 March 2020). "India-South Africa series called off due to COVID-19 threat". The Hindu. Retrieved 13 March 2020.
- ^ "Coronavirus: Attari border ceremony to be conducted without public presence". Livemint. Press Trust of India. 6 March 2020. Retrieved 6 March 2020.
- ^ Singh, Jitendra Bahadur (14 March 2020). "Upcoming Padma Awards ceremony postponed in wake of coronavirus outbreak". India Today. Retrieved 14 March 2020.
- ^ "Coronavirus impact: Statue of Unity closed for public; ASI shuts all monuments". Business Standard. 17 March 2020. Retrieved 15 May 2021.
- ^ "ASI monuments, including Red Fort and Qutub Minar, opened for public; footfalls barely touch 100". Times Now. 7 July 2020. Retrieved 8 July 2020.
- ^ "IIFA 2020 cancelled due to coronavirus scare, fresh date to be announced soon". Hindustan Times. 6 March 2020. Retrieved 6 March 2020.
- ^ Jha, Lata (15 March 2020). "Coronavirus scare in India: All film, TV, web shoots cancelled". Livemint. Retrieved 15 March 2020.
- ^ Laghate, Gaurav (25 March 2020). "Video streaming services like Netflix, Hotstar suspend HD streaming on cellular networks". The Economic Times. Retrieved 15 May 2021.
- ^ "Home | Ministry of Health and Family Welfare | GOI". mohfw.gov.in. Retrieved 17 April 2020.
- ^ Biswas, Soutik (20 November 2020). "India coronavirus: How a group of volunteers 'exposed' hidden Covid-19 deaths". BBC. Retrieved 19 April 2021.
- ^ Biswas, Soutik (18 August 2020). "Coronavirus: How many Covid-19 deaths is India missing?". BBC. Retrieved 19 April 2021.
- ^ Pulla, Priyanka (4 August 2020). "India Is Undercounting Its COVID-19 Deaths. This Is How". The Wire. Retrieved 19 April 2021.
- ^ Krishnan, Murali (26 April 2021). "Coronavirus: Is India counting all COVID deaths?". Deutsche Welle. Retrieved 27 April 2021.
- ^ Langa, Mahesh (18 April 2021). "COVID-19 deaths in Gujarat far exceed government figures". The Hindu. Retrieved 19 April 2021.
- ^ Ara, Ismat (18 April 2021). "In Ghaziabad and Other Districts, Data on Ground Disproves UP's 'Zero COVID Deaths' Claim". The Wire. Retrieved 19 April 2021.
- ^ "In Kolkata and Chennai, Actual COVID Death Toll May Be Four Times Higher". The Wire. New Delhi. 31 May 2021. Retrieved 1 June 2021.
Further reading
Articles
- Sharma, Vyoma Dhar (9 May 2021), 'Each Burning Pyre Is a Screeching Horror' – Notes From India's COVID Frontline, The Wire Science
- Kelkar, Ram (9 May 2021), "India's COVID-19 Crisis Is Due to Its Collective Failure, Blaming Others Doesn't Help", The Wire
Government
- COVID-19 Vaccines. Operational Guidelines. (Updated as on 28 December 2020). (PDF), Ministry of Health and Family Welfare, Government of India., archived from the original (PDF) on 26 February 2021
- COVID-19 Vaccine. Communication Strategy. (PDF), Ministry of Health and Family Welfare, Government of India., archived from the original (PDF) on 29 January 2021
- Science and Technology Efforts in India on COVID-19. Exclusive Edition on Vaccines & Immunisation. (PDF), Vigyan Prasar (An Autonomous Organisation of Department of Science & Technology, Government of India., 31 January 2021
- Science and Technology Efforts in India on COVID-19. Exclusive Edition on Outreach Initiatives. (PDF), Vigyan Prasar (An Autonomous Organisation of Department of Science & Technology, Government of India., 28 February 2021
External links
| Wikimedia Commons has media related to COVID-19 pandemic in India. |
- COVID-19 on MyGov.in – Government's portal for COVID-19
- "District Map of CoViD-19 in India". fieldmaps.in. Retrieved 2 May 2020.
- Vigyan Prasar COVID-19 newsletters. 36 Issues between 10 April 2020 to 11 May 2021.
- COVID-19 pandemic in India playlist on YouTube – COVID-19 Management videos by the Ministry of Health and Family Welfare
- Prasad, R.; Perappadan, Bindu Shajan; Shelar, Jyoti (2020). George, P.J. (ed.). The Pandemic Notebook (PDF). The Hindu.
A handy guide from The Hindu on understanding the coronavirus pandemic and staying protected against COVID-19
- Khaiwal, Ravindra; Mor, Suman. "Kids, Vaayu & Corona: Who wins the fights (A comic series for COVID-19 awareness)" (PDF). www.mohfw.gov.in. MoHFW, Government of India.
- "Coronavirus in India: Latest Map and Case Count". www.covid19india.org. A crowdsourced initiative. (javascript required)
- "Reuters Covid-19 Tracker India. Current charts of infections, deaths, vaccinations". Reuters.
Information
Article COVID-19 pandemic in India in English Wikipedia took following places in local popularity ranking:
- 21 place in 2020-03-11
- 26 place in 2020-03-12
- 24 place in 2020-03-13
- 20 place in 2020-03-14
- 11 place in 2020-03-15
- 8 place in 2020-03-16
- 7 place in 2020-03-17
- 10 place in 2020-03-18
- 7 place in 2020-03-19
- 6 place in 2020-03-20
- 6 place in 2020-03-21
- 7 place in 2020-03-22
- 4 place in 2020-03-23
- 4 place in 2020-03-24
- 3 place in 2020-03-25
- 3 place in 2020-03-26
- 3 place in 2020-03-27
- 5 place in 2020-03-28
- 6 place in 2020-03-29
- 6 place in 2020-03-30
- 6 place in 2020-03-31
About the page
Presented content of the Wikipedia article was extracted in 2021-06-12 based on https://en.wikipedia.org/?curid=63265538